November 29, 2022
Note: This resource is intended to be useful both as a standalone document, as well as the third part of Business Group on Health’s Value-Based Purchasing Guide. Click the link to access additional parts related to other elements of employer value-based purchasing strategy.
Primary care is often employees’ first touchpoint with the health care system perhaps beside the pharmacy counter, making it a key component of any value-based purchasing strategy. While primary care doesn’t directly drive the burdensome health care costs in an employer’s plan, it does directly influence many other downstream impacts of care (e.g., referrals, labs, imaging, prescriptions, chronic disease management, preventive screenings, mental health). One estimate suggests that 90% of health care spending can be influenced by primary care, even though it only accounts for 5%-6% of overall spending. For this reason, primary care is especially well-suited to value-based reimbursements tied to overall health outcomes or total cost of care.6
Primary care physicians (PCPs) and their care teams are often in the most effective position to provide holistic care and refer patients to high-quality, efficient specialists. Additionally, given that fee-for-service reimbursement rates for primary care are relatively low compared to other types of intensive or specialty care, it is possible that primary care providers will receive a modest increase in payment through a value-based arrangement, allowing them to invest in tools to improve care and better manage total cost of care, leading to overall savings for the plan.
What Is Value-Based Primary Care?
In value-based primary care arrangements, PCPs take responsibility to improve the health of a population that is assigned to them. This stands in contrast to the traditional FFS system that simply reimburses a flat fee for services delivered. In value-based primary care models, PCPs and their teams are enabled to innovate and practice in ways that optimizes population health and patient experience, coordinating across other provider groups, integrating mental health and embracing virtual care delivery where appropriate.
The FFS system hamstrings PCPs by making any actions they take (e.g., hiring extra nursing staff to follow-up with patients after a visit) to improve quality of care outside a traditional billable visit a financial drain for their practice. This in turn forced payers to provide those services outside the PCP office through care management programs often disconnected from data available to physicians and their nurses. By migrating to value-based payment arrangements, PCPs are able to fund services, such as integrated electronic health records providing actionable data, pre-visit triage and post-visit check-ins, to ensure a streamlined experience for patients. This experience includes selecting the most appropriate provider on the care team for each patient, adhering to evidence-based guidelines during the visit and using technology to better communicate with patients instead of relying on office visits or phone calls.
Advanced primary care models have another advantage using technology and data: They empower PCPs to refer patients to appropriate specialty care. This not only steers patients to high-quality care, it also can drive down the total cost of care. Every model listed below seeks to use effective referrals to steer patients to high quality, efficient specialty care to drive total cost of care reductions.
Direct Primary Care (DPC)
Practices in the DPC model do not accept fee-for-service payments; instead, they are reimbursed through full capitation. With these completely upfront payments tied to performance guarantees on total cost of care and patient outcomes, DPC practices can invest in services that others cannot. For example, upfront payments enable DPC practices to do broader outreach to patients before they come in for doctor visits, invest in technology to expand access to virtual care for their patients and better manage chronic conditions at home by connecting patients to social services in their community. DPC practices can decide where to spend time and resources based on the severity of their patients’ conditions without having to over-schedule quick patient visits to make FFS payment targets – a process dubbed “Hamster Wheel Medicine.”7
DPC offerings are emerging into the employer market and existing primary care partners to employers have acquired DPC practices, opening up the opportunity to employers even further.8
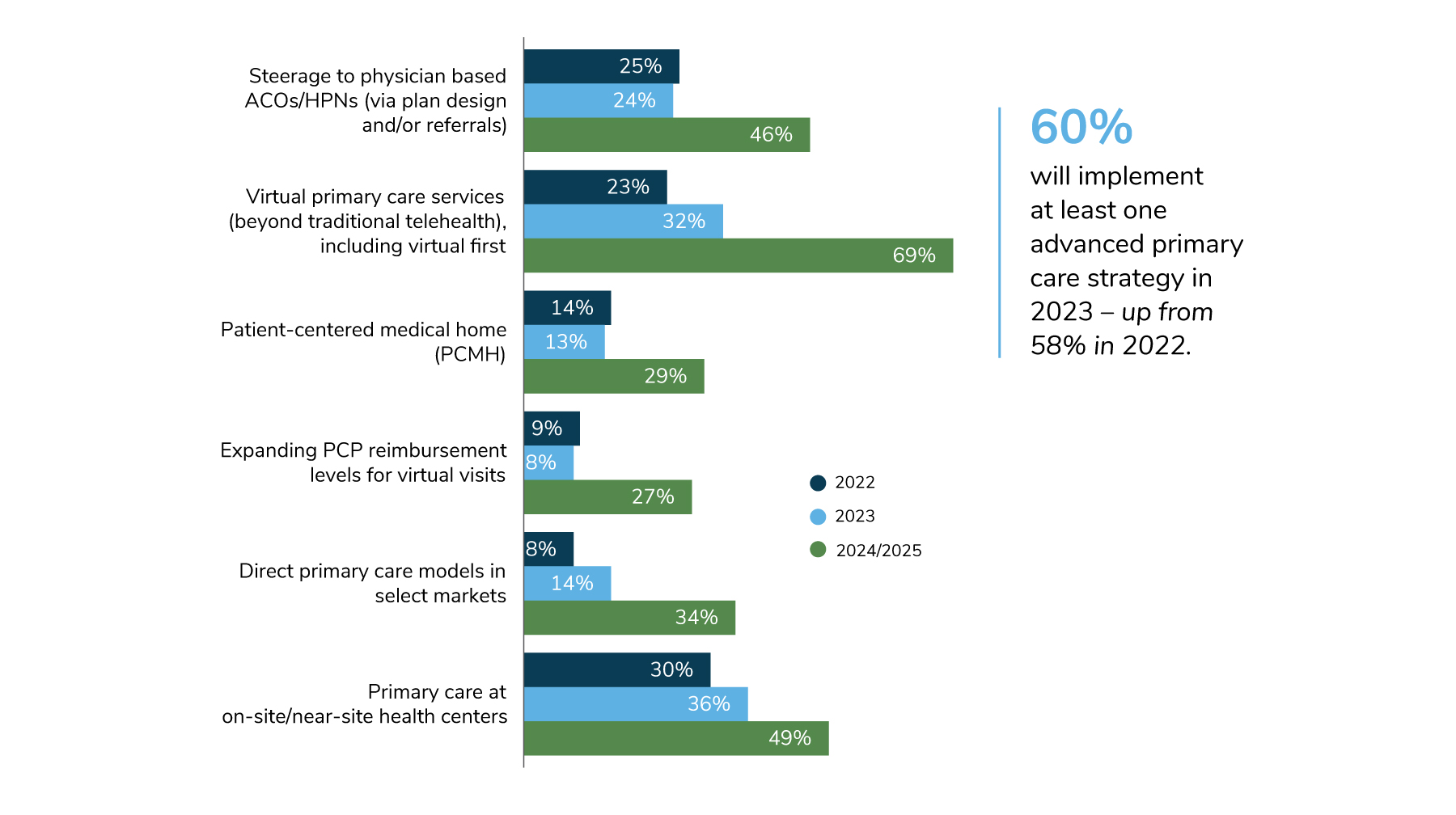
Source: 2023 Large Employers’ Health Care Strategy and Plan Design Survey
Enhanced On-site or Near-site Clinics with Primary Care
Many employers work with provider partners to increase the scope of services offered in their on-site and near-site clinics, including holistic primary care, pharmacy and mental health. Many of these providers are reimbursed through value-based arrangements or capitation. The convenience of making a full suite of primary care services available near the worksite may improve productivity and increase access to underutilized services like mental health care and preventive care. By having control over quality measures through directly contracting with these providers, employers are better able to address a variety of core issues impacting health care quality and waste, such as emergency room overutilization, low preventive screening rates, mental health inclusion and affordability of services.
Virtual-first Primary Care
The virtual-first primary care model encourages patients to start their health care experience with virtual care, then steers them to in-person care only for those interactions that cannot be carried out effectively through virtual means. Primary care providers who operate in this model deliver health care services virtually first, then facilitate patients arriving at the “last mile” of care through scheduling of in-person services and referrals to specialists – some who may also operate virtually.
Growth of Virtual Primary Care
According to the 2023 Large Employers’ Health Care Strategy and Plan Design Survey, virtual primary care services, including a “virtual first” model, are slated to experience the most potential growth between 2022 (23%) and 2025 (69%) – an upward swing of 46 percentage points.
By centralizing the “front door” to primary care through a virtual-first care team, it may be easier to also create value-based payment models for this care, rather than doing so across hundreds of in-network primary care providers in a given geography. Employers have long been interested in tying virtual health payments to value, especially amid concerns about the potential for duplicative costs if virtual care visits don’t fully address a patient’s needs and an additional in-person visit becomes necessary. By tying payment for virtual services to value and outcomes, providers are in a better position to direct patients to where their care is best delivered for a particular circumstance and condition. FFS payment for virtual care may lead to over-utilization (if providers find that revenue gains are possible by encouraging easily accessible virtual visits) or under-utilization (if providers steer patients in-person because virtual care is reimbursed less so than in-person visits.)
As virtual health capabilities increase to allow for additional communication between patients and physicians and at-home care outside traditional telehealth visits proliferate, value-based payment will be all the more necessary to enable the infrastructure necessary to implement these new methods of care. See the Business Group’s Virtual Care Guide for more information.
Primary Care Focused Accountable Care Organizations (ACOs)
ACOs are responsible for the health outcomes and cost of care for population of patients attributed to them. ACO provider networks include specialists that aren’t traditionally associated with primary care, but by centering the ACO’s leadership and financial accountability on primary care providers, they have the ability to improve health and control costs through referral patterns, while benefiting financially themselves. See Section 4 – Accountable Care Organizations and High Performance Networks for more information on ACOs.
An analysis of the first 5 years of the Medicare ACO program finds that primary care led ACOs tend to have higher quality scores compared to their counterparts led by hospital systems.9 ACOs led by primary care groups have also seen greater success in controlling total cost of care in Medicare compared to those run by hospitals. One study of 2019 Medicare ACO data found that savings associated with ACOs that were primary care led were seven times higher than for those ACOs with partial or full hospital ownership.10 Hospital-led ACOs tend to have dueling incentives to reduce total cost of care to meet ACO-related financial goals as well as to increase hospital utilization to drive FFS revenue. Primary care providers in an ACO do not make additional money when a patient goes to the hospital, making them theoretically more likely to steer patients to more efficient sites of care to the best of their ability.
Conclusion
Principles for an Optimal Primary Care Experience
The Business Group’s Executive Committee on Value Purchasing and the Health Innovations Forum, comprised of leading employers and industry experts, created an employer-focused resource called Principles for an Optimal Primary Care Experience, which lays out in more detail what employers should look for when assessing primary care partners.
Primary care is the crux of health care delivery and impacts significant downstream health services, making it an increasingly important component of most value-based arrangements. Many payment reform options are available that may enable primary care providers to expand their ability to lengthen visits for patients who need it, increase access to virtual care when appropriate, proactively outreach to people about preventive services and supercharge their ability to coordinate care and connections to social services.
Employer Recommendations
- 1 | Ask your health plan and provider partners how they are leveraging primary care to improve their value-based care strategy. Questions should include:
- How are you managing referrals to guide plan members to high- quality, efficient specialists?
- What is your geographic coverage in markets of interest?
- What is your track record on quality metrics like completion of recommended preventive services and cost mitigation?
- Are you able to refer to employer- sponsored vendor programs?
- What are your virtual care capabilities?
- What level of risk are you able to contract for in value-based reimbursement arrangements? Note that some are able to take on full capitation, while others may be only prepared for shared- savings arrangements .
- For virtual-first models, how are you making referrals to in-person care? Do you employ specialists who deliver in-person care, contract with them or simply direct employees to specialists in their PPO network?
- How is care coordinated between primary care and specialists?
- 2 | Consider using plan design incentives to reduce cost barriers to accessing primary care in value-based arrangements, given their importance to the success of ACOs, HPNs and DPC practices. This can include reducing cost-sharing for primary care providers delivering value-based care via on-site clinics or virtual modalities. Pre-deductible coverage of primary care is not currently possible through health savings account eligible plans, but it is possible through other plan designs, and ongoing legislative efforts are in place to increase employer flexibility to cover additional primary care services at the beginning of the plan year.
- 3 | Assess growing opportunities for direct contracting with virtual care providers delivering comprehensive primary care services. Several vendors have emerged in the past 3-5 years that are able to provide a large set of primary care services for employees through on-site, near-site and virtual clinics. Some 32% of large employers will contract for virtual primary care services in 2023 and another 36% cover primary care in on-site and near-site centers.11 In-person care strategies will require a larger employee population in a given geography than virtual care, but providers with brick-and-mortar offices will be able to deliver a wider set of services.
- 4 | As the set of services that PCPs can deliver grows, consider which resources in your benefits ecosystem could be eliminated to avoid duplication. In a given geography with a strong primary care partnership, an employer may be able to eliminate additional vendor contracts that focus on increasing preventive services, for example, because that can be handled by the primary care system.
- 5 | Determine which quality metrics are important to you and use them as a starting point for which performance goals will be used in value-based contracting with primary care provider groups. Quality metrics for primary care will focus more on utilization of preventive care across your population, but referral management and cost mitigation are significant areas of opportunity to make an impact on total cost of care. Direct billing for primary care services is a small portion of health care spend, but primary care providers have a large impact on total cost of care through referral patterns.
- 6 | Assess how primary care providers have integrated mental health care. This can dramatically increase utilization rates of evidence-based mental health services compared to expecting plan members to navigate spotty provider networks on their own.
More Topics
Articles & Guides- 1 | Centers for Medicare & Medicaid Services. Performance Year 2021 APM Performance Pathway: CMS Web Interface Measure Benchmarks for ACOs. Quality Payment Program. Accessed October 11, 2022. https://qpp-cm-prod-content.s3.amazonaws.com/uploads/1306/Performance%20Year%202021%20APM%20Performance%20Pathway-CMS%20Web%20Interface%20Measure%20Benchmarks%20for%20ACOs.pdf
- 2 | The Leapfrog Group. Preventing and Responding to Patient Harm. Leapfrog Ratings. Accessed October 11, 2022. https://ratings.leapfroggroup.org/measure/hospital/preventing-and-responding-patient-harm
- 3 | Agency for Healthcare Research and Quality. About CAHPS. July 2022. Accessed October 11, 2022. https://www.ahrq.gov/cahps/about-cahps/index.html
- 4 | Conti R et al. Projections of US Prescription drug spending and key policy implications. JAMA Health Forum. 2021;2(1). https://jamanetwork.com/journals/jama-health-forum/fullarticle/2776040. Accessed November 8, 2022.
- 5 | Business Group on Health. Emerging Trends in Cancer Care. October 25, 2021. https://www.businessgrouphealth.org/resources/emerging-trends-in-cancer-care. Accessed November 8, 2022.
- 6 | Golden W et al. Changing how we pay for primary care. New England Journal of Medicine Catalyst. November 20, 2017. https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0326. Accessed November 8, 2022.
- 7 | Bitton A et al. Off the hamster wheel? Qualitative evaluation of a payment-linked patient-centered medical home (PCMH) pilot. The Milbank Quarterly. 2012 Sep; 90(3): 484–515. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3479381/. Accessed November 8, 2022.
- 8 | Primary Care for Boeing’s Mesa Employees. Iora Health. Accessed on February 9, 2022. https://ioraprimarycare.com/boeing/
- 9 | Bleser W, et al Half a decade in, Medicare accountable care organizations are generating net savings: Part 1. Health Affairs Blog. September 20, 2018. https://www.healthaffairs.org/do/10.1377/forefront.20180918.957502/full/. Accessed November 8, 2022.
- 10 | Sullivan G, Feore J. Physician-led accountable care organizations outperform hospital-led counterparts. Avalere. October 15, 2019. https://avalere.com/press-releases/physician-led-accountable-care-organizations-outperform-hospital-led-counterparts. Accessed November 8, 2022.
- 11 | Business Group on Health. 2023 Large Employers’ Health Care Strategy and Plan Design Survey. https://www.businessgrouphealth.org/resources/2023-plan-design-health-care-delivery-system. Accessed November 8, 2022.
- 12 | Lapsey H. The Better Benefit Stack. 2018 Oliver Wyman Health Innovation Journal. https://health.oliverwyman.com/2019/03/the-better-benefit-stack.html
- 13 | Centers for Medicare & Medicaid Services. Medicare Shared Savings Program Continues to Grow and Deliver High-Quality, Person-Centered Care Through Accountable Care Organizations. CMS Newsroom. January 26, 2022. https://www.cms.gov/newsroom/press-releases/medicare-shared-savings-program-continues-grow-and-deliver-high-quality-person-centered-care-through. Accessed November 8, 2022.
- 14 | O’Reilly K. Doctor participation in ACOs, medical homes grows amid pandemic. American Medical Association. December 7, 2021. https://www.ama-assn.org/practice-management/payment-delivery-models/doctor-participation-acos-medical-homes-grows-amid. Accessed November 8, 2022.
- 15 | Avalere. MSSP Sees Continued Growth in Downside Risk ACOs. January 21, 2020. https://avalere.com/insights/mssp-sees-continued-growth-in-downside-risk-acos. Accessed November 8, 2022.
- 16 | Mechanic R et al. The 2018 Annual ACO Survey: Examining the Risk Contracting Landscape. Health Affairs Forefront. April 23, 2019. https://wwwhealthaffairs.org/do/10.1377/forefront.20190422.181228/full/. Accessed November 8, 2022.
- 17 | Business Group on Health. 2023 Large Employers’ Health Care Strategy and Plan Design Survey. https://www.businessgrouphealth.org/resources/2023-large-employers-health-care-strategy-and-plan-design-survey
- 18 | Business Group on Health. 2023 Large Employers’ Health Care Strategy and Plan Design Survey. https://www.businessgrouphealth.org/resources/2023-plan-design-health-care-delivery-system.
- 19 |Elkins K. Lowe's free surgery program helps cut costs, benefit employees. Charlotte Business Journal. March 30, 2016. https://www.bizjournals.com/charlotte/blog/outside_the_loop/2016/03/lowe-s-free-surgery-program-helps-slice-costs.html. Accessed November 8, 2022.
-
IntroductionValue-based Purchasing Employer Guide: Introduction
-
Executive SummaryValue-based Purchasing Employer Guide: Executive Summary
-
Part 1Definitions and Measures of Value in Value-based Purchasing
-
Part 2Value-based Reimbursement Strategies
-
Part 3Value-based Primary Care
-
Part 4Accountable Care Organizations and High-Performance Networks
-
Part 5Centers of Excellence
-
Part 6Value-based Virtual Care
-
Part 7Value-based Care Engagement Strategies
This content is for members only. Already a member?
Login
![]()
