November 29, 2022
Currently, in the U.S. health care system, most medical services are paid for using a set fee with no regard to necessity, outcomes or patient experience. This “fee-for-service” (FFS) reimbursement system incentivizes providers to do more, inflating costs of care, while also hampering them from doing things that could improve patient care but aren’t considered reimbursable services, such as answering patient e-mails or consulting expert specialists.
Value-based payments for health care services generally transfer a portion of financial risk to health care providers based on the health outcomes and quality of service that they deliver. If providers in value-based contracts perform well on cost and quality metrics, they stand to benefit financially through bonus payments and other means.
The intention of changing the way that providers are paid is to drive changes in the way that they care for their patient population. When providers are paid to keep people healthy rather than to perform medical services, prevention becomes a top priority, inappropriate or unnecessary surgeries become a money loser rather than a significant source of revenue, and coordination of care across settings becomes all the more important. Patients, employers and providers stand to benefit when value-based payments enable high-quality care.
Employers considering value-based payment strategies should take several steps to determine if and how they should proceed.
1| Become familiar with value-based contracting payment approaches to drive improvements in care for plan members.
Moving away from FFS reimbursements can take many forms. Some work around the edges of FFS through “shared savings” arrangements that largely keep the FFS system intact but result in bonus payments to providers who are able to improve quality and mitigate costs. Others are more transformative in how they transfer financial risk to providers, which may be more effective in bringing about positive change in delivery of care. Unfortunately, however, fewer provider groups are willing to take on financial risk, as it requires greater transformation of care delivery and business practices.
Employers should also consider how different payment arrangements will impact their finances through the year. FFS payments are not ideal for most health care services, but they do result in claims that are fairly predictable throughout the year. Some value-based reimbursement approaches will require employers to keep money in reserve to make bonus payments to providers that achieve positive outcomes and mitigate overall costs. Others, like bundled payments, which cover most services across a defined episode of care, will likely be more costly up front, but result in downstream savings over time.
2| Consider which value-based care model best addresses the health care needs of your population
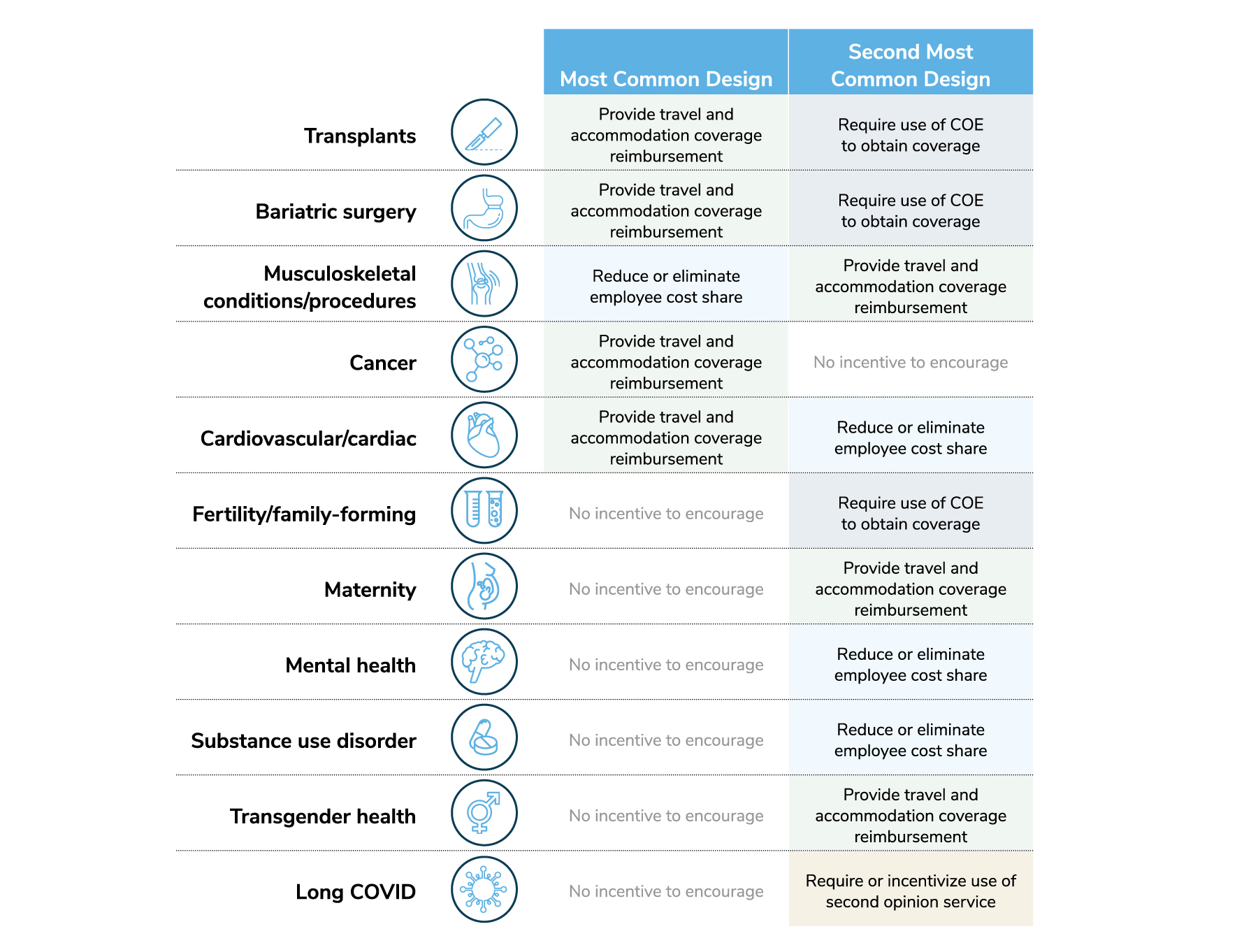
Value-based contracting can be as focused as one particular procedure or as broad as encompassing the entirety of care for a large population. Employers should consider what problem they’re trying to solve with pursuing a value-based purchasing strategy. Seeing a spike on costs of care for cancer? A Center of Excellence (COE) with very high-quality and positive outcomes for patients may be appropriate. Do you have a geography where employee health outcomes are lagging others, or one with particularly high cost of care? Then a high-performance network (HPN) or accountable care organization (ACO) may be the best approach.
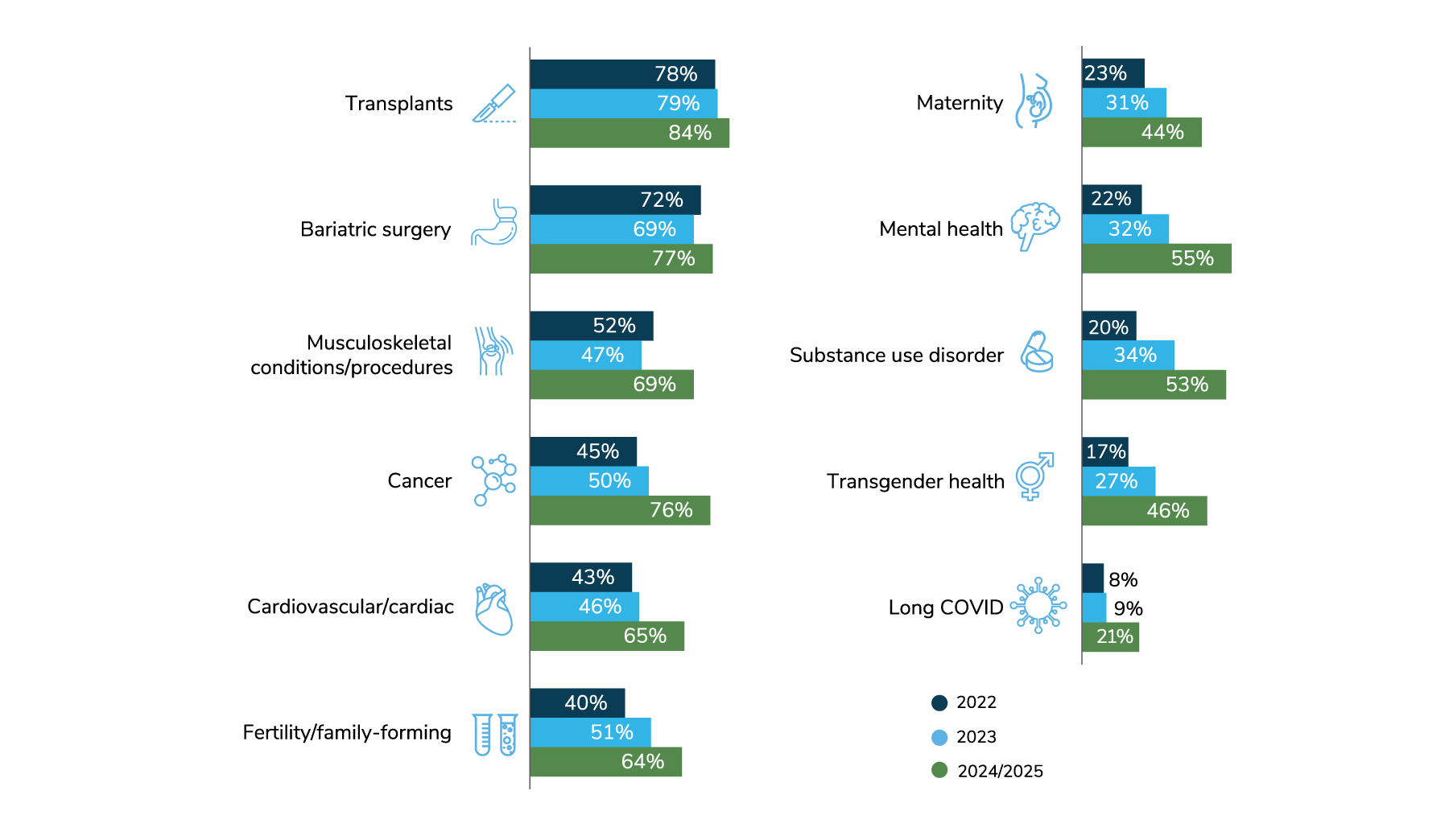
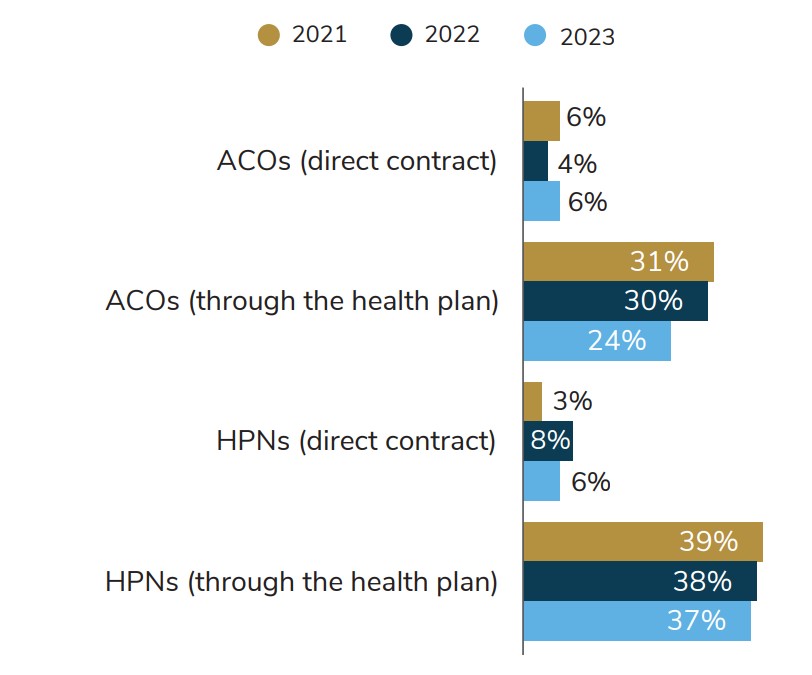
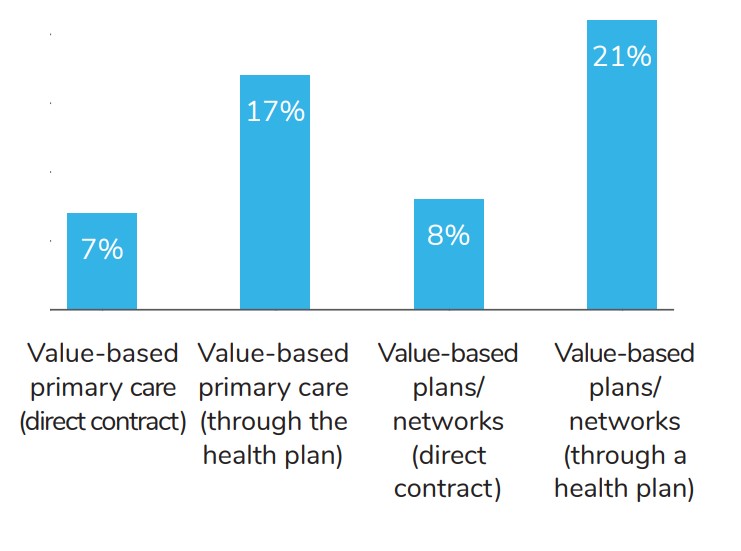
All graphs in this section are from the 2023 Large Employers’ Health Care Strategy and Plan Design Survey.
3| Identify partners that can help you implement value-based reimbursements to drive improvements in care
Value-based purchasing requires a partnership between employers, providers, and third parties who facilitate the contracting and implementation – most often a health plan, though new companies are emerging that operate outside of traditional models.
Selecting provider partners will depend on the delivery model that employers are considering, such as a surgery COE or a population-wide network. Assess quality and cost variation in care for your targeted patient population and decide which thresholds of performance are necessary for you to consider a partnership with providers in that specialty or geography.
Partners to facilitate contracting and implementation generally fall into three categories:
- Health plans, which have established relationships with providers and wide geographical coverage for several value-based care approaches.
- Companies that curate COEs and HPNs in select geographies across the U.S. These companies may be able to customize their contracting approaches in ways that health plans cannot, but it does mean that employers have to take on another vendor .
- Third-party administrators that specialize in facilitating direct contracting between employers and providers. Direct contracting gives employers more flexibility in value-based contracting but requires additional time and resources to execute.
4| Determine how you will steer employees and dependents to value-based care providers
Plan members will only benefit from value-based care if they see providers who are delivering it. Additionally, provider groups will generally only enter value-based contracts (and take on associated financial risk) if there is some mechanism for steering plan members to them.
Directing employees to providers in value-based arrangements can run the gamut from simply communicating the benefit of seeking care from participating providers to restricting coverage to only include care from those providers. Employers will need to decide how aggressively they will use engagement and plan design levers to direct where their plan members seek care.
5| Monitor performance of value-based contracts and make adjustments as necessary
Effective value-based purchasing arrangements take time to achieve results, especially for those covering an entire population of plan members. Employers should understand going into a value-based purchasing strategy that, in most cases, this is a long-term approach to improving care for their plan members. Therefore, it is important to monitor provider performance over time to make sure that goals are being met and to build in intervals during contracting where conditions can be adjusted if necessary.
Conclusion
Health care costs are higher than ever with no visible improvement in life expectancy or overall health. The health care system is built on a payment model that rewards providers for doing more care, rather than appropriate care, and the FFS model does little to incentivize providers to keep people healthy and out of the system in the first place. Self-insured employers have purchasing power they can use to accelerate the move away from FFS, which benefits their employees and their families.
More Topics
Articles & Guides-
IntroductionValue-based Purchasing Employer Guide: Introduction
-
Executive SummaryValue-based Purchasing Employer Guide: Executive Summary
-
Part 1Definitions and Measures of Value in Value-based Purchasing
-
Part 2Value-based Reimbursement Strategies
-
Part 3Value-based Primary Care
-
Part 4Accountable Care Organizations and High-Performance Networks
-
Part 5Centers of Excellence
-
Part 6Value-based Virtual Care
-
Part 7Value-based Care Engagement Strategies
