August 25, 2021
Looking for the latest data?
Check out our 2024 Large Employer Health Care Strategy Survey, released in August 2023.
Key Takeaways
- Seventy percent of large employers are concerned about health equity within their health and well-being initiatives.
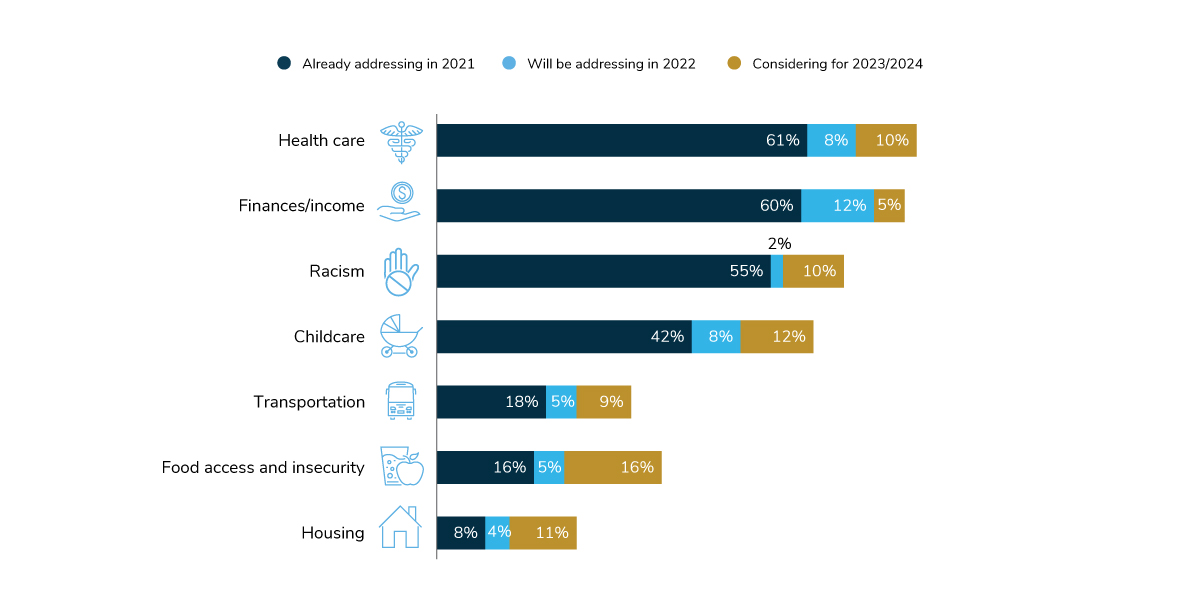
- Health care access and finances/income are the top two social determinants of health (SDOH) addressed by employers, while childcare and food access/insecurity will receive increased focus from more employers in 2022, 2023 and 2024.
- In 2022, over 80% of employers will address health inequities in three main ways: through family-forming benefits (82%), expanding benefits to support a neurodiverse population (81%) and offering or expanding coverage of transgender health care benefits (80%).
Health Equity in 2021
For the first time, the survey asked employers how they are addressing health equity within their benefit plans. The social justice movement, coupled with inequities brought to light during the COVID-19 pandemic, sparked increased focus among employers and employees alike, with employers committed to ensuring that all employees have access to quality health care and benefits that meet their diverse needs. In fact, 7 in 10 surveyed employers show a level of concern about health equity within their health and well-being initiatives. This section presents examples of how employers are attempting to address these concerns through various strategies.
Social Determinants of Health (SDOH)
Employers are initiating programs and benefits to address the circumstances that employees and their families are born into and live, which have an impact on employees’ ability to live healthy and fulfilling lives. Tackling underlying social and economic challenges can influence regular health habits, overall well-being and even one’s mortality and may bring health care closer to systemic change (Figure 2.1).
Health Care
The most common SDOH that employers are addressing is health care, with 61% of employers already focusing on it in 2021 and another 18% committed to doing so by 2024. Having adequate access to quality health care involves not only the number of doctors in a community, but also access to health insurance, ability to afford out-of-pocket costs, availability of transportation to health care providers and physician availability. It is no surprise that many employers are looking to solve these issues on a systemic level, as these variables are at the very core of their health care strategy.
Two ways employers are addressing access to health care are: 1) making health care coverage more affordable and thus attainable for employees earning lower wages and 2) expanding telehealth and telemental health services to employees living in communities with an insufficient number of providers and/or lack of reliable transportation to medical appointments.
Finances/Income
Another critical SDOH is finances/income, which is associated with health outcomes, including life expectancy. A majority of employers have focused on this factor; 60% are addressing income as a SDOH in 2021 and another 17% plan on doing so in the next 2-3 years. Those earning lower incomes often face challenges accessing health care, as they have a harder time affording deductibles, copayments and other health care expenses.
The first step in addressing income as a SDOH is by paying a living wage, a strategy some survey respondents indicated that they have implemented. Other employers are offsetting premiums for lower-income employees and placing additional funds in their health savings accounts (HSAs). And still others are offering financial benefits and programs to support employees on their financial well-being journey, such as initiatives that help employees build emergency savings funds.
Racism
Nearly 67% of large employers will be actively addressing racism as a SDOH in the next 3 years. Racism impacts physical, mental and financial well-being profoundly, creating and reinforcing health inequities across the globe. Employers can play a role in eliminating racism in their workplaces and the communities in which they operate.
According to survey respondents, actively partnering with equity, diversity and inclusion teams, employee resource groups and internal leaders is a common starting place to address racism. Other ways employers can advance health equity is to assess racial and ethnic disparities that occur in their health plan or care covered by the plan, with a focus on outcomes, engagement and access to care and cultural consciousness. Employers can also work with their partners to promote cultural competency training among health care professionals to ensure a diverse, culturally competent network of health care providers from health plans and vendors.
Childcare
Access to affordable childcare impacts families in two ways: providing a means for an employee to work and earn a wage while their child is being cared for and giving children a jump-start in their development and education, which can have a lasting effect on their well-being later in life. Currently, 42% of employers are focused on childcare as a social determinant of health; another 20% will turn their attention to this by 2024.
Common ways to aid working parents and caregivers is to subsidize the cost of childcare or even provide discounted childcare directly on-site. Some are also providing backup childcare to help employees manage unexpected gaps in care. Because the pandemic has greatly limited childcare availability, employers may want to consider reserving a certain number of spots at on-site or local childcare centers for employees earning lower incomes.
Transportation
Without reliable and safe transportation, employees may be denied regular access to healthy foods, medical care and pharmacies. They may even be unable to report for work, potentially impacting their ability to earn a full wage. While only 18% of employers are actively addressing transportation in their communities, another 14% will begin to do so in the next few years.
As noted in Part III, many employers with a traveling Centers of Excellence (COE) program will pay for travel and assistance to higher-quality facilities. Some employers are subsidizing transportation to work and medical appointments to help offset the expense. Ridesharing has provided new opportunities for employees to commute to work.
Food Access
Food access is under a watchful eye from many employers; while only 16% of employers are actively focused on this area, an additional 21% are planning to direct their attention here in the future, making it the largest area of potential growth of any SDOH. The absence of nutritious and affordable foods (“food deserts”) and the abundance of high-calorie dining options (“food swamps”) in communities have been well-documented as having a negative impact on diet quality, fruit and vegetable consumption and overall obesity rates.
Some employers are working to solve this problem by making nutritious foods more readily available on-site, and sometimes, subsidizing groceries, ready-made meals or meal vouchers for employees.
Housing
For some Americans, affordable housing may be out of reach. In addition, some housing options may be substandard and lead to an increase in health risks associated with asthma, cardiovascular events, physical illness and psychological trauma. Only 8% of employers are addressing housing instability in 2021, with another 15% planning to focus on it by 2024.
Examples shared by employers include providing down payment assistance, homebuyer workshops and advocacy support for employees facing poor housing conditions. Some employers are even going so far as to form community partnerships to address challenges in the locales where employees live and work.
Addressing Health Equity in Health Benefit Plans
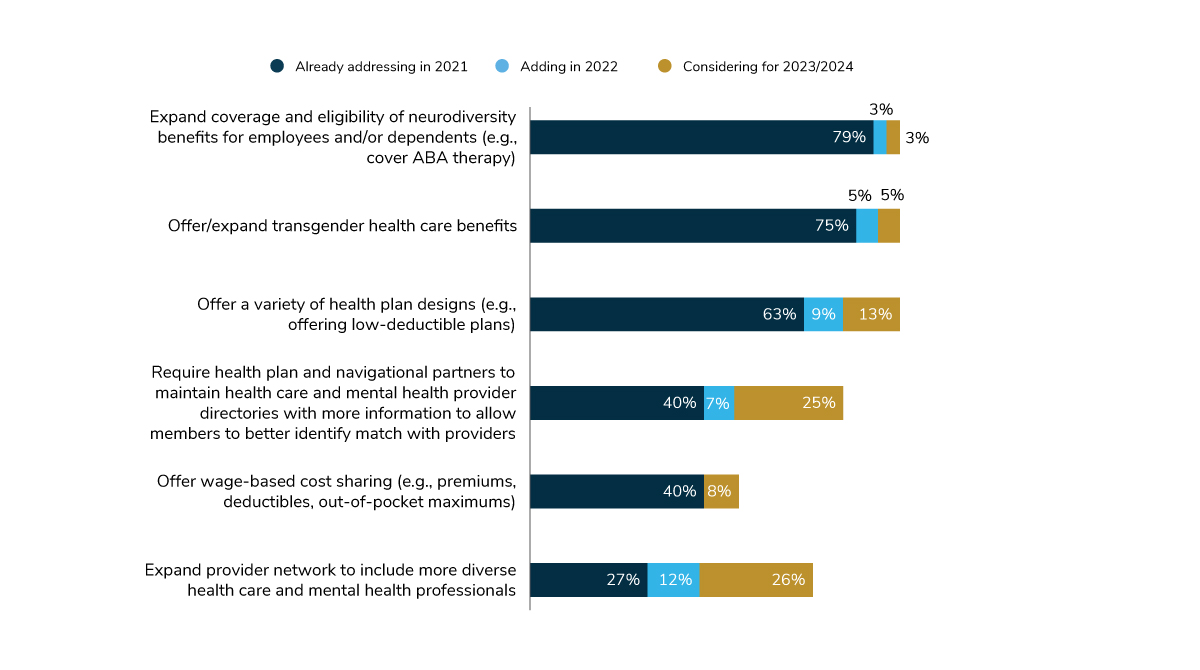
In 2021, the majority of employers are working to ensure that employees have equal access to quality health care and are treated respectfully during health care interactions. As seen in Figures 2.2 and 2.3, the top focus areas are family-building benefits, as well as coverage for neurodiversity benefits and transgender procedures/supports.
Family-building Benefits
Disparities in maternal/birth parent care are well-documented, and supporting all paths to parenthood is now commonly seen as fundamental to inclusive benefits. Therefore, it’s no surprise that 82% of large employers will implement at least one tactic to reduce health inequities within family-building benefits by 2022. The most common way is to identify high-risk pregnancies among under-resourced populations, an approach that will be used by 47% of employers. Forty-four percent of employers are expanding coverage to treat postpartum depression (PPD).
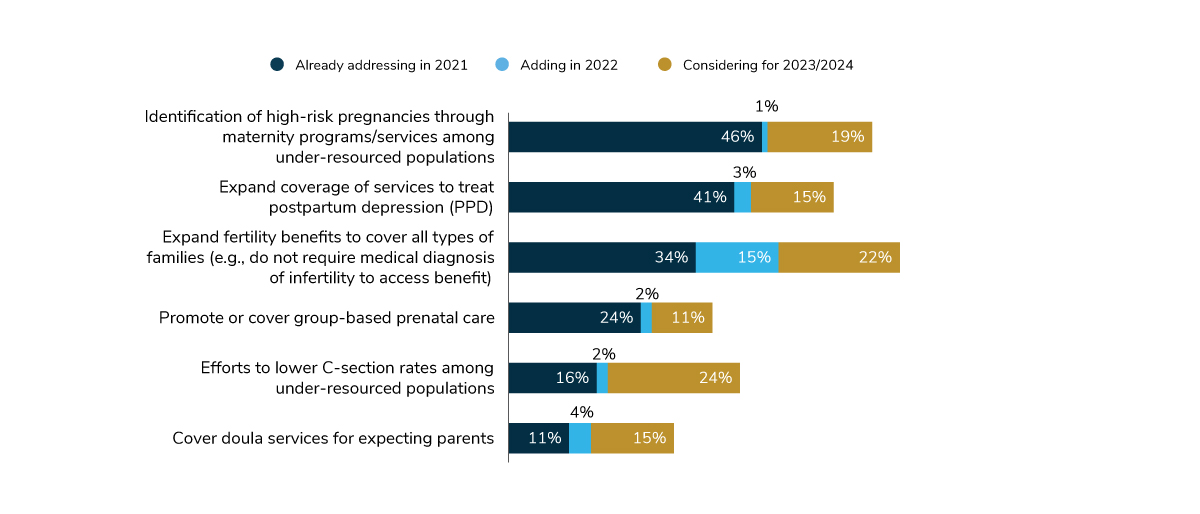
However, employers are setting their sights on two other sources of inequities for 2024, signaling the most substantial areas of growth for this area. Expanding fertility benefits to cover all types of families will more than double in just 3 years (from 34% in 2021 to 71% in 2024). While a focus on lowering C-section rates among under-resourced populations isn’t common today (with just 16% of employers doing so), an additional 26% of employers plan to make this a priority in the next 1-3 years.
Neurodiversity
Neurodiversity is an area of health equity that has long been a focus, as evidenced by the fact that 8 in 10 employers have an established program in place in 2021. While the emphasis historically was on supporting employees and dependents with autism spectrum disorder, some employers are expanding their benefits to aid those with attention deficit hyperactivity disorder (ADHD), dyslexia, social anxiety disorders and other conditions that may affect occupational skillsets and personal interactions.
Transgender Health Care Benefits
Employers are also expanding coverage to support transgender employees. Seventy-five percent of employers will offer or expand transgender health care benefits in 2021, and an additional 10% will do so in 2022-2024.
Some employers are offering transgender coverage for the first time. Others are deeming additional procedures as eligible for coverage and/or bumping up the lifetime maximum benefit so employees are provided with more funds to support their transition.
Patient Affordability of Health Insurance
As seen in Figure 2.1, finances/income is one of the top social determinants of health being actively addressed by employers. This issue affects health equity as it relates to the affordability of health insurance coverage. Despite the heavy subsidization of employer-sponsored care (see Part IV), some employees may not earn enough to afford monthly premiums or out-of-pocket costs in addition to housing, transportation, food and other necessities.
This finding also relates to the downward trend of employers offering full replacement consumer-directed health plans. In 2022, many employers (72%) will offer a variety of health plan types to appeal to a wider swath of incomes (Figure 2.3). This means that employees who struggle with deductibles and coinsurance levels may now have access to other plan types with lower deductibles, making it easier for employees to receive affordable health care. Additionally, 48% of employers will adjust or tier cost-sharing by wage, so premiums, deductibles and out-of-pocket maximums are at the lowest levels for those earning the least.
Provider Networks
Importantly, employers are looking to their providers (physical and mental health practitioners) and vendor partners (such as health plans, navigational services and well-being programs) to do their part in supporting health equity efforts. Currently, there are an inadequate number of providers with a specific expertise (e.g., gender transition) or demographic background (race/ethnicity). While it is important to increase the number of diverse providers within networks, it is just as important that all providers practice care that is culturally competent.
In addressing these concerns, one step is to better identify providers within the provider directory who have specific characteristics; 40% of employers are currently requiring the health plan and other partners to take this extra step, while another 32% aim to put it in place by 2024. The challenge with this requirement is with the data; not all plans/vendors have the ability to solicit and gather this information, and not all providers are willing to have these attributes added to their practice profile.
A more systemic way to achieve employees’ desires for a more diverse pool of providers is to expand the provider network to include more individuals with characteristics absent or lacking from the current network. In 2021, 27% of employers will be expanding their networks with diversity in mind; that number will more than double to 65% by 2024.
-
Introduction2022 Large Employers’ Health Care Strategy and Plan Design Survey
-
Full Report2022 Health Care Strategy and Plan Design Survey: Full Report
-
Executive Summary2022 Health Care Strategy and Plan Design Survey: Executive Summary
-
Chart Pack2022 Health Care Strategy and Plan Design Survey: Chart Pack
-
Infographic2022 Health Care Strategy and Plan Design Survey: Infographic
-
Part 1Employer Perspectives on the Health Care Landscape
-
Part 2Health Equity Within Health and Well-being Initiatives
-
Part 3Employers and the Health Care Delivery System
-
Part 4Health and Pharmacy Plan Design
-
Part 5Health Care Costs and 2022 Priorities
More Topics
Data Insights
This content is for members only. Already a member?
Login
![]()
