November 14, 2023
Although obesity has increased almost everywhere around the globe, its rise in the U.K. has been particularly alarming and has increased steadily throughout the last three decades. As a result, the U.K. has the fourth highest prevalence of obesity in Europe, behind only Turkey, Malta and Israel. 7
The WHO European Region, which includes 53 countries, is affected most by noncommunicable disease (NCD) related morbidity. Recent estimates suggest that overweight and obesity cause more than 1.2 million deaths across the WHO European Region every year, the fourth highest cause after high blood pressure, dietary risks and tobacco and correspond to more than 13% of total deaths.7
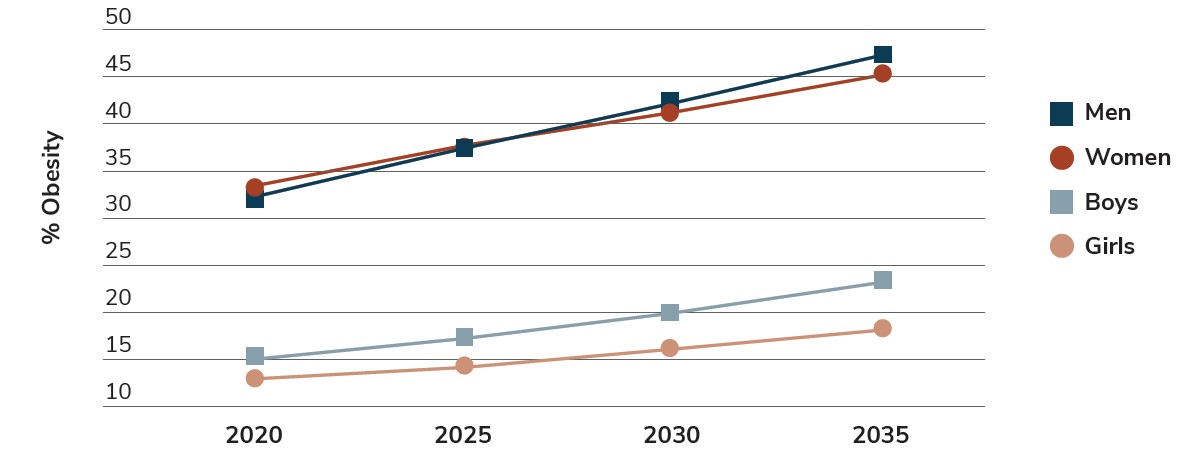
Future projections from the Cancer Research of U.K. estimate that more than 21 million or more U.K. adults will be obese by 2040, or 4 in 10 of the entire U.K. adult population. If the current trend continues, the number of people living with obesity could overtake those with a healthy weight as early as the late 2020s (Figure 5.1).9
U.K. Spotlight5
- 25.9% of adults are obese.
- Men are more likely than women to be overweight or obese (68.6% of men compared to 59.0% of women).
- People aged 45-74 are most likely to be overweight or obese.2,7
- The Northeast and North Cumbria region has the highest prevalence of obesity at 13%, whereas Southwest London has the lowest prevalence with 7%.
Source: World Obesity Federation: World Obesity Atlas 2023.
Employer Opportunity
There are huge, short- and long-term repercussions associated with the rise of obesity in the U.K. that directly impact the workplace and society as a whole. Yet, according to Business Group on Health’s Global Weight Management Survey, few employer respondents in the U.K. consider it a top priority. Employers should take time to better understand the impact of obesity on their workforce’s health, well-being and productivity and determine what steps they can take to help mitigate the impact of obesity and overweight.
Tackling Obesity with An Eye Toward Equity
In historically marginalized areas in the U.K., the prevalence of obesity or being overweight is 9% higher.2 Also, overweight and obesity are the leading behavioral factors that increase disability risk, causing 7% of total years lost due to disability (YLDs) in the region. The U.K. government's most recent figures show that compared to 2016, the percentage of adults who are overweight or living with obesity went up in their categorized groups for “mixed ethnic” (from 53.9% to 59.5%) and “other ethnic” (from 58.9% to 66.2%).5
Employer Opportunity
It would be beneficial for employers to analyze their weight management programs to ensure that they are being deployed equitability. Employers should also include obesity and overweight explicitly in Diversity, Equity, Inclusion and Belonging (DEIB) practices. In addition, employers should audit the availability of support and services through the National Health Service (NHS) and fill gaps where possible.
Cost and Impact of Overweight and Obesity
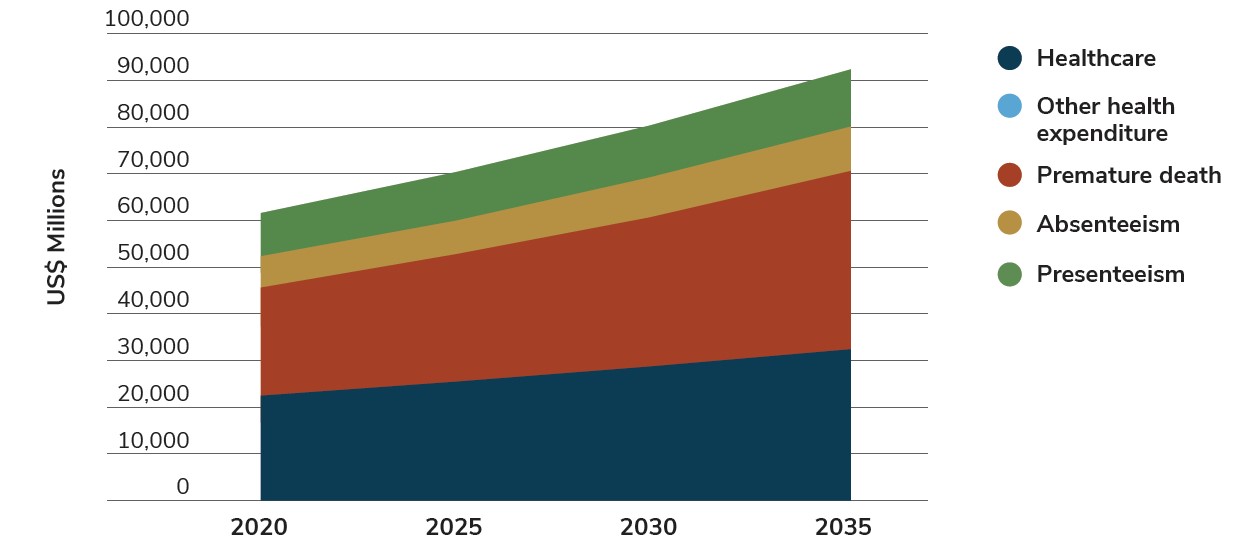
The cost of obesity and overweight in the U.K. is high, making the cost of taking no action extraordinary. Every government since 1992 has identified obesity as a major problem, and recent estimates show an annual cost of obesity at 1-2% of GDP, a figure likely to only increase.3 Specifically, in the U.K., it is estimated to cost the NHS £6.5 billion a year, with this amount set to rise to over £9.7 billion each year by 2050.18
Table 1.1: Impact of Overweight
|
|
Health care impact of BMI ≥ 25kb/m2, US$ million |
Total economic impact of BMI ≥ 25kb/m2, US$ million |
Estimated GDP US$ billion |
Impact of BMI ≥ 25kb/m2 on GDP |
|---|---|---|---|---|
|
2020 |
22,482 |
61,530 |
2,612 |
2.4% |
|
2025 |
25,421 |
70,247 |
3,056 |
2.3% |
|
2030 |
28,749 |
80,294 |
3,383 |
2.4% |
|
2035 |
32,422 |
91,761 |
3,792 |
2.4% |
Source: World Obesity Federation: World Obesity Atlas 2023.
In 2022, the national health budget was approximately £283 billion, or 11.4% of GDP (gross domestic product).12 Spending on preventive care was £35.1 billion in 2021, more than double the cost in 2020, due to the government’s response to COVID-19 (Figure 5.2).12 In 2022, the government announced a £20 million research boost to develop new medicines and digital tools, which have been shown to help people shed 20% of their weight.18
Source: World Obesity Federation: World Obesity Atlas 2023.
Although patients trust physicians as information sources on diet and weight loss, studies suggest that the management of nutrition-related disorders is hindered by insufficient medical education and training.13 Also, although there are clear care pathways and clinical guidelines for evidence-based practice, there remains no single stakeholder willing to take overall responsibility for obesity care.14
Weight loss surgery, such as bariatric or metabolic surgery, is available by the NHS if the person living with obesity has a BMI of 40 or more or a BMI between 35 and 40 and an obesity- related condition that might improve with weight loss (such as type 2 diabetes or high blood pressure); tried other weight loss methods; and agrees to long-term follow-up after surgery, including making healthy lifestyle changes and attending regular checkups.10
Business Group on Health’s Global Weight Management Survey reveals that weight management programs are covered through the health plan by less than half of employer respondents in the U.K. (n=14). This includes outpatient services/nutrition counseling, prescription drugs and bariatric surgery. Top reasons for employers not offering weight management programs in the U.K. include existing coverage by the national health plan, lack of demand, cost of services and the employer’s need to reset the narrative regarding obesity being a lifestyle issue.
Employer Opportunity
With long wait times plaguing the NHS, employers should audit their available weight management initiatives with an eye toward outcomes. Business Group on Health’s Global Weight Management Survey shows that very few employers in the U.K. have data or outcome information related to weight management, creating an opportunity to move toward more evidence-based solutions.
Addressing Rising Rates of Obesity and Overweight: Government Interventions
In 2021, the government of the U.K. announced the Health and Care Bill, the first of its kind around the world to ban all paid advertising of unhealthy food products on online platforms. Other proposed government strategies to address ongoing concerns about the downstream impact of obesity in the U.K. include prohibiting stores from placing unhealthy food in prominent locations such as the entrances, checkouts and at the end of aisles, banning advertising of food high in fat, salt and sugar before 9 pm and stopping multibuy promotions, such as “buy one, get one free,” for unhealthy food.
In addition to environmental and societal policies, there is a growing interest in pharmacological options, especially as revolutionary weight loss drugs enter the market. Britain plans to launch pilot programs in efforts to enhance equitable access to weight loss drugs. Administration through the NHS is limited to hospital settings and can be given only by a doctor’s referral. Furthermore, the prescription can only be used for a maximum of 2 years. To decrease obesity’s financial burden on the NHS, the country is exploring ways to make the most effective therapies accessible via general practitioners and specialty pharmacies.
Employer Opportunity
While Business Group on Health’s Global Weight Management Survey results indicate that employers rate the quality of weight management services either very good (14%) or good (21%) in the U.K., the highest of the five countries surveyed, there is still work to be done. Employers have a unique opportunity to review government coverage and identify gaps on what to cover, taking into consideration private pay options.
The Workplace’s Impact on Overweight and Obesity
Public Health England estimates that an organization employing 1,000 people loses more than £126,000 per year from obesity-related health issues. Additionally, studies show that 131 million working days are lost every year due to sickness absences (with 31 million due to musculoskeletal conditions, themselves frequently worsened by weight complications), and the costs to employers and taxpayers are around £22 billion a year.4 Every 12 months, more than 300,000 people have to leave work and claim health-related benefits.4 While not all of these claims are due to obesity, it does have a dramatic impact on the well-being of the workforce.7
Employer Opportunity
Due to the undeniable evidence of the workplace’s impact on an employee’s well-being, coupled with the evaluation of workplace environments post-COVID, employers should review policies that influence sedentary practices. This could include mindful design of the workplace infrastructure with an eye to promoting spontaneous walking opportunities or bolstering flexible working options
Obesity Stigma
Since obesity is a topic that many people have underlying opinions about, it can lead to further stigmatization for those with obesity. This stigma can reinforce barriers to understanding its causes, prevalence and access to treatment.11 According to Business Group on Health’s weight management survey, weight stigma is high in the U.K., and 7% of employers state it is severe.
Employer Opportunity
Business Group on Health’s Global Weight Management Survey shows that 47% of employers in the U.K. do not address weight stigma in their programs (n=20). Employers may want to consider developing a culturally conscious weight management program that is not solely focused on food and diet. A holistic approach is crucial so that the people you are trying to support do not feel stigmatized or alienated from the workplace. To implement such an approach, review current workplace well-being communication practices and programs to ensure they are supportive, inclusive, culturally conscious and compassionate.
In fact, the increasing prevalence of individuals living with obesity and overweight in the U.K., and throughout the world, will require a holistic approach to interventions. The workplace implications are vast, as is the interconnection of obesity with other conditions, including mental health issues. Not only is taking action an imperative from a population health perspective, it also serves as a mechanism to curtail associated health care costs and other worsening long-term impacts affecting economic well-being and overall societal health.
Obesity and Overweight in the United Kingdom
More Topics
Articles & Guides- 1 | ITV. Government's fear to fight obesity burdening the NHS. April 19, 2023. https://www.itv.com/thismorning/articles/governments-fear-to-fight-obesity-burdening-the-nhs. Accessed June 5, 2023.
- 2 | Baker C. Obesity statistics. House of Commons Library. January 12, 2023. https://commonslibrary.parliament.uk/research-briefings/sn03336/. Accessed June 6, 2023.
- 3 | Metcalfe S, Sasse T. Tackling obesity: Improving policy making on food and health. Institute for Government. April 2023. https://www.instituteforgovernment.org.uk/sites/default/files/2023-04/tackling-obesity.pdf. Accessed June 2, 2023.
- 4 | Government Business. The workplace consequences of obesity. https://governmentbusiness.co.uk/features/obesity-%E2%80%93-what-are-consequences-your-department. Accessed June 5, 2023.
- 5 | Office for Health Improvement and Disparities. Overweight adults. May 24, 2023. https://www.ethnicity-facts-figures.service.gov.uk/health/diet-and-exercise/overweight-adults/latest. Accessed June 2, 2023.
- 6 | OECD. Obesity and the economics of prevention: Fit not fat - United Kingdom (England) Key Facts. September 2010. https://www.oecd.org/els/health-systems/obesityandtheeconomicsofpreventionfitnotfat-unitedkingdomenglandkeyfacts.htm. Accessed June 5, 2023.
- 7 | Townsend N, Heinen M, Rakovac I, et al. WHO European regional obesity report 2022. World Health Organization Regional Office for Europe. 2022. https://apps.who.int/iris/bitstream/handle/10665/353747/9789289057738-eng.pdf. Accessed June 2, 2023.
- 8 | Burger L, Fick M. Weight-loss drugs pilot to begin in U.K. amid uncertainty over Wegovy launch. Reuters. June 7, 2023. https://www.reuters.com/business/healthcare-pharmaceuticals/uk-explore-wider-access-obesity-drugs-50-million-pilot-2023-06-06/. Accessed June 10, 2023.
- 9 | Smith J. New analysis estimates over 21 million U.K. adults will be obese by 2040. Cancer Research U.K. May 19, 2022. https://news.cancerresearchuk.org/2022/05/19/new-analysis-estimates-over-21-million-uk-adults-will-be-obese-by-2040/. Accessed June 9, 2023.
- 10 | NHS. Weight loss surgery. April 14, 2020. https://www.nhs.uk/conditions/weight-loss-surgery/. Accessed June 8, 2023.
- 11 | Bajorek Z, Bevan S. Obesity stigma at work: Improving inclusion and productivity. Institute for Employment Studies. 2020. https://www.employment-studies.co.uk/system/files/resources/files/Obesity%20Stigma%20at%20Work%20-%20Improving%20Inclusion%20and%20Productivity_0.pdf. Accessed June 10, 2023.
- 12 | Office for National Statistics (ONS). Healthcare expenditure, U.K. Health Accounts provisional estimates: 2022. May 17, 2023. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthcaresystem/bulletins/healthcareexpenditureukhealthaccountsprovisionalestimates/2022. Accessed June 5, 2023.
- 13 | Ganis L, Christides T. Are we neglecting nutrition in U.K. medical training? A quantitative analysis of nutrition-related education in postgraduate medical training curriculums. Nutrients. March 16, 2021; 13(3): 957. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8000414/. Accessed June 6, 2023.
- 14 | Capehorn MS, Haslam DW, Welbourn R. Obesity treatment in the U.K. health system. Curr Obes Rep. September 2016; 5(3):320-6. https://pubmed.ncbi.nlm.nih.gov/27352180/. Accessed June 10, 2023.
- 15 | Bulut M. Key statistics on the NHS. NHS Confederation. May 2, 2023. https://www.nhsconfed.org/articles/key-statistics-nhs. Accessed June 10, 2023.
- 16 | Holmes J. Tackling obesity: The role of the NHS in a whole-system approach. The King’s Fund. July 2021. https://www.kingsfund.org.uk/sites/default/files/2021-07/Tackling%20obesity.pdf. Accessed June 3, 2023.
- 17 | Department of Health and Social Care. New drugs pilot to tackle obesity and cut NHS waiting lists. June 6, 2023. https://www.gov.uk/government/news/new-drugs-pilot-to-tackle-obesity-and-cut-nhs-waiting-lists. Accessed June 10, 2023.
- 18 | Department of Health and Social Care. New obesity treatments and technology to save the NHS billions. November 27, 2022. https://www.gov.uk/government/news/new-obesity-treatments-and-technology-to-save-the-nhs-billions. Accessed June 10, 2023.
- 19 | Business Group on Health. Global Weight Management Survey. April 7, 2023. https://www.businessgrouphealth.org/resources/global-weight-management-survey. Accessed June 20, 2023
This content is for members only. Already a member?
Login
![]()
