November 14, 2023
In India, almost 23% of men and 24% of women have a BMI in the overweight or obesity range- many more in urban areas than in rural areas (33.2% of women and 29.8% of men compared to 19.7% of women and 19.3% of men, respectively).
Source: World Obesity Federation: World Obesity Atlas 2023.
The number of adults with a BMI in the overweight or obesity range has increased approximately 3-4% since 2015-2016.1 A recent study projects that the prevalence of overweight may double, and obesity may triple, by 2040.2
While the prevalence of obesity and overweight is higher in urban areas, rural areas are rapidly catching up, particularly those that are in closer proximity to large cities. In these areas, there is greater consumption of convenience foods and a higher likelihood of nonfarm occupations. Obesity and overweight have also started to shift from the wealthy to lower and middle socioeconomic groups in these areas, especially among those who eat less diverse diets.11 In fact, lack of dietary diversity plays a role in both under- and overnutrition in both high and low socioeconomic households throughout India.12
Employer Opportunity
Increase access to a wide variety of food choices in canteens and cafeterias, limiting packaged, processed and convenience items and subsidizing healthier options. Consider offering take-home options to employees to increase dietary diversity outside work and educate employees about the importance of a healthy, varied diet.
Cost and Impact of Overweight and Obesity
In 2019, the total cost of obesity in India, including direct (i.e. health care) and indirect (i.e. lost productivity) costs was, in U.S. dollars, $23.24 billion, approximately 0.8% of the gross domestic product (GDP).3 By 2060, the total costs are projected to be $839 billion in U.S. dollars, or 2.49% of the GDP, the third highest of 161 countries studied.4
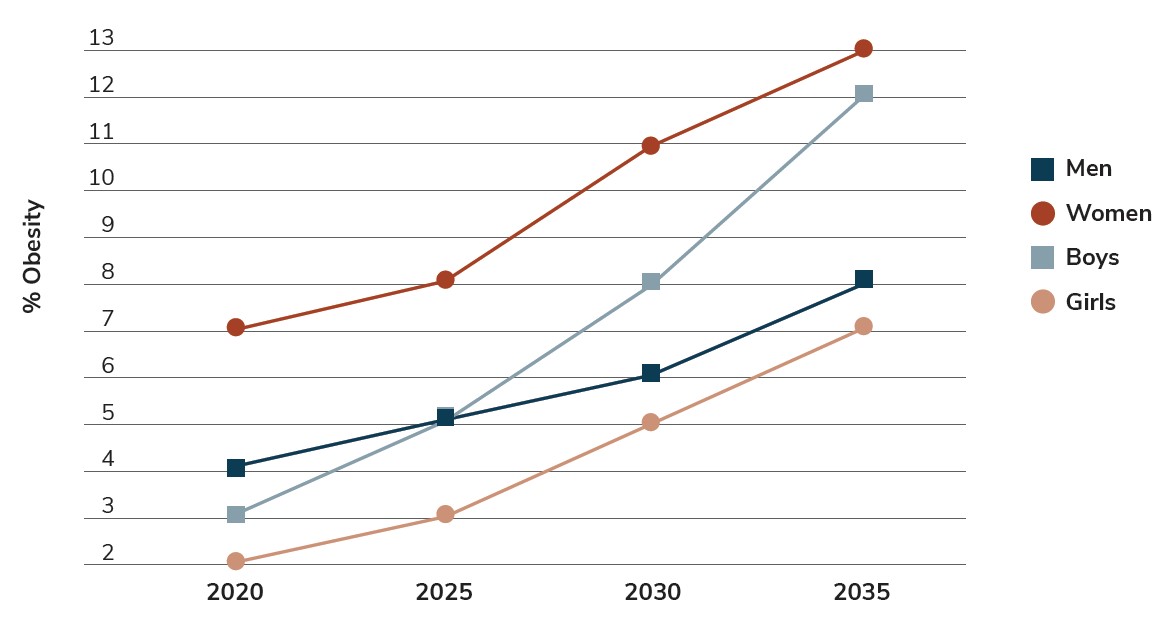
Table 3.1: Projected Trends in the Prevalence of Obesity
|
|
Health care impact of BMI ≥ 25kb/m2, US$ million |
Total economic impact of BMI ≥ 25kb/m2, US$ million |
Estimated GDP US$ billion |
Impact of BMI ≥ 25kb/m2 on GDP |
|---|---|---|---|---|
|
2020 |
2,456 |
31,603 |
2,645 |
1.2% |
|
2025 |
3,785 |
50,696 |
3,815 |
1.3% |
|
2030 |
5,730 |
81,527 |
5,206 |
1.6% |
|
2035 |
8,430 |
129,326 |
7,117 |
1.8% |
Source: World Obesity Federation: World Obesity Atlas 2023.
The projected global economic impact of overweight, including productivity loss at work, from 2020 to 2035 is shown in Figure 3.2. The rise in obesity and overweight in India has occurred alongside significant economic growth over the last couple of decades. This has led to a more sedentary lifestyle, with a greater number of people in white-collar office jobs than in blue-collar or agricultural jobs where they expend more energy.5 Fast food has become more readily available as globalization has increased in the country,6 and the sales of packaged and processed food almost doubled from 2012 to 2018.7,8 Other contributing factors, depending on gender, area of the country and level of development, include rising age, access to motorized transport, increased TV watching and reductions in smoking.9 A recent study showed that 4 out of 10 people living in India do not get the recommended amount of physical activity. This is particularly true among women and those living in urban areas.10
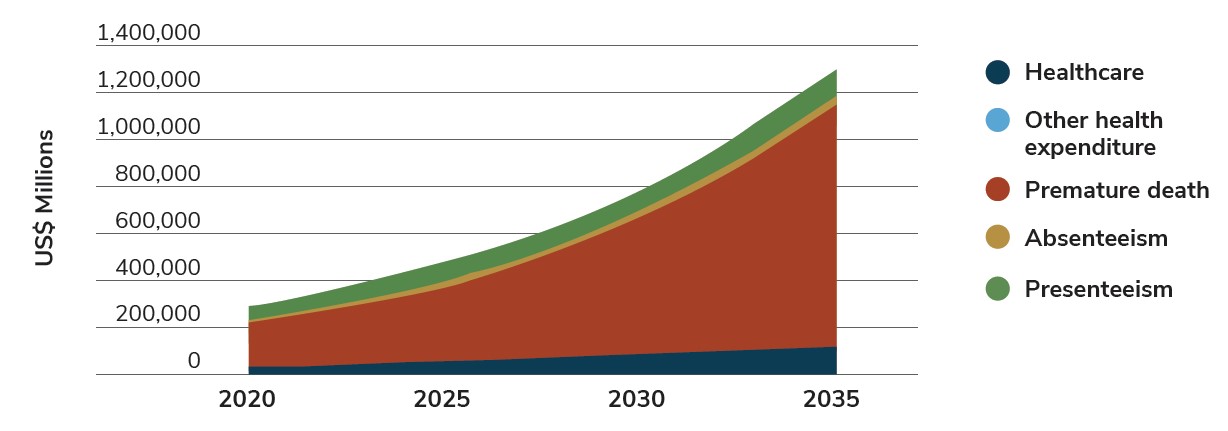
Source: World Obesity Federation: World Obesity Atlas 2023.
The prevalence of non-communicable diseases (NCDs) such as heart disease and diabetes has risen in India due to urbanization and globalization, causing an increase in traditional cardiovascular disease risk factors such as obesity. 13 36 Unfortunately, there has been a lack of appropriate response to NCDs in the public sector due to a number of factors: “a lack of risk-factor and disease surveillance systems, poor access to drugs and diagnostic services, limited public financing or insurance, and human resource limitations.”14 Therefore, most treatment takes place in tertiary hospitals in the private system.14 In one study, 50-70% of those seeking treatment for NCDs did so through private health care services.13 In 2017, NCDs made up approximately 47% of deaths, with 55% of those in urban areas.15 Almost two-thirds of these deaths were among people under the age of 70. Furthermore, hospitalization rates due to NCDs rose from 29% in 2004 to 38% ten years later.13 Economic costs related to NCDs are high; a 2018 review showed that most studies estimated that the cost burden related to NCDs accounted for 5-10% of GDP.16
Because of these issues, more attention needs to be paid to obesity, a key risk factor for non-communicable diseases. Education and access to opportunities for physical activity are two strategies that could help.
Employer Opportunity
Provide various ways for employees to access physical activity, including on-site or near-site fitness centers, discounted workout classes, virtual offerings, step challenges and incentives to engage in movement. Education about the importance of physical activity may be beneficial as well. This is especially important for employees in offices or similar settings, where they may be more sedentary than workers in other locations.
Lack of knowledge about their own health status is another issue. For example, more than half of people with diabetes are unaware of their diagnosis.18 Employers can provide screening programs for diabetes and risk factors for other NCDs through on-site clinics, health checks and preventive care benefits to ensure that employees get the care they need to be healthy and productive at work.
There is some debate about the BMI cutoff for overweight and obesity in India and throughout Asia. Some researchers have proposed that a BMI of 23kg/m2 for overweight and a BMI of 25 kg/m2 or above for obesity, which is lower than the World Health Organization cutoffs of 25 kg/m2 and 30 kg/m2, respectively. This is because health conditions have a tendency to occur at lower BMIs in this population.19 One potential reason for this is that Asian populations often have 3-5% higher body fat than white Europeans of the same BMI.20,21 South Asians in particular have even higher levels of body fat, particularly related to abdominal obesity.21-23 Some early evidence shows that lifestyle changes may have a slow but positive impact among the population living with obesity and overweight at these proposed lower BMI standards.24
Obesity Stigma and Mental Health Concerns
There are few studies on weight stigma in India. One out of three women studied with a BMI over 35 kg/m2 reported stigma and discrimination, as did 18% with a BMI over 30 kg/m2 and 5% with a BMI over 25 kg/m2. Fifty-nine percent to 95% of these women reported dissatisfaction with their weight, again with dissatisfaction increasing as weight increased.25 Another study looked at the correlation between stigma, mental health and disordered eating patterns among individuals receiving services at a bariatric clinic. Those who reported high levels of stigma were more likely to be women; to report bingeing, overeating, or grazing; and to have mental health diagnoses.26
Research on weight stigma in the U.S., Western Europe and Australasia (which includes Australia, New Zealand and some neighboring islands) may be applicable to India. Studies show that stigma changes health behaviors for the worse and can lead to depression, anxiety and suicidality. Furthermore, emerging research in low- and middle-income countries suggests that it is highly distressing and may lead to similar outcomes.27 In 2023, only 7% of employers responding to a survey said that they had programs to address weight stigma in the workplace, even though 40% said it was moderately severe.17
More work has to be done on the relationship between people with obesity and mental health in general among the Indian population. A study of patients at a bariatric clinic with a BMI over 40 kg/m2 without any co-morbidities, or a BMI over 35 kg/m2 with significant medical problems, found that 33.33% of respondents had a mental health condition, most commonly depression and dysthymia. Close to a fifth of respondents had a substance use disorder. However, the population studied was fairly small (n=60).29 Another study of adolescents in Kolkata showed that obesity was correlated with depression, anxiety and stress.30 On the other hand, research conducted among patients at two hospitals in South India showed no correlation between overweight or obesity and risk for depression, except among individuals under the age of 40.30
As of 2022, the Insurance Regulatory and Development Authority of India (IRDAI) has mandated that insurance companies cover mental health under their policies. However, only hospitalization of at least 24 hours is required, not out-patient services such as counseling.31,32 Employers can support their employees’ mental health by providing comprehensive benefits that cover outpatient counseling and medication provisions, as well as employee assistance programs (EAPs) and other solutions, such as mindfulness, stress management and resilience programs.
Employer Opportunity
Weight stigma and bias is associated with a host of negative consequences for people with obesity, including avoidance of physical activity, delaying of preventive care and increased risk of chronic conditions. Employers can address stigma by incorporating weight bias training into workplace trainings, asking employees about their experiences with bias during focus groups and ensuring that health and well-being materials are free from stigmatizing language and imagery.28
Addressing Rising Rates of Obesity and Overweight in India: Trends in Employer Coverage, Policy Developments and Interventional Approaches
Bariatric surgery was first performed in India in 1999, and now is offered in both private and public hospitals. Since then, surgeries have increased annually, but a stigma remains. Starting in 2019, “bariatric and metabolic surgery has been included in health insurance by the Insurance and Regulatory Development Authority of India (IRDAI) for the treatment of obesity.” This is likely to increase the number of surgeries taking place in the country as well as awareness of the procedure.33 The Obesity and Metabolic Surgery Society of India recommends that adults ages 18-65, who have tried repeatedly to lose weight and have a BMI greater than 37.5 kg/m2 without any co-morbidities, and a BMI of 32.5 kg/m2 with any related co-morbidities, be considered for bariatric surgery. Those older than 65 or younger than 18 may be considered in certain circumstances, such as severe co-morbidities in older adults or after attainment of puberty and pediatric certification in those younger than 18.34
Orlistat is currently approved for pharmacological use for weight management in India. It may also lead to improvements in cardiovascular risk factors, blood pressure and serum lipid levels, although risk factors related to oily stools and increased defecation are possible, among others. Medication is only recommended once lifestyle interventions have not been successful in reducing weight.24
The Executive Committee of the Endocrine Society of India has proposed medical nutrition therapy (MNT) -- “a process and provision of nutritional assessment, counselling, advice (dietary, nutritional and culinary) and follow-up for prevention and/or management of obesity by a qualified or trained health care provider” -- to support dietary changes in people living with obesity or overweight. However, MNT is not covered by insurance in the country and individuals must pay out of pocket. Furthermore, doctors generally aren’t aware of its importance, and there aren’t an adequate number of trained nutritionists. MNT also isn’t generally individualized to the needs of the patient. Overall, the society recommends that a multidisciplinary team that incorporates diet, exercise, and pharmacotherapy as needed be involved in supporting patients living with obesity and overweight.24
Data from Business Group on Health’s Global Weight Management Survey show that weight management programs offered through health plans include outpatient services/nutrition counseling and bariatric surgery.17 Employers who don’t offer weight management programs most often cite lack of demand, cost or coverage through the public health care system as the reasons for not including those programs.
Employer Opportunity
Employers can consider offering access to medical nutrition therapy through health insurance plans, and/or access to on-site nutritionists or health coaches that help employees manage their weight. However, due to the lack of trained nutritionists in the country, it’s important to be realistic about what may be possible.
In conclusion, while the Indian government and society has historically been more focused on problems related to underweight and communicable diseases, obesity, overweight and NCDs are rapidly increasing throughout the country, leading to a greater burden on families, the health care system and employers. Employers can do their part to mitigate this rising tide through private supplemental health insurance by providing access to evidence-based treatment options for obesity where available, educating employees about health risk factors for NCDs, offering on-site services to bolster what’s offered in the public system, addressing weight bias through training, focus groups and non-stigmatizing materials, and ensuring access to mental health services and programs through their supplemental plan offerings.
Obesity and Overweight in India
More Topics
Articles & Guides- 1 | Government of India. National Family Health Survey (NFHS-5)- 2019-2021. Compendium of Fact Sheets. http://rchiips.org/nfhs/factsheet_NFHS-5.shtml. Accessed February 15, 2023.
- 2 | Luhar S, Timæus IM, Jones R, et al. Forecasting the prevalence of overweight and obesity in India to 2040. PLoS ONE. 2020;15(2)
- 3 | Okunogbe A, Nugent R, Spencer G, Ralston J, Wilding J. Economic impacts of overweight and obesity: current and future estimates for eight countries. BMJ Glob Health. 2021;6(10)
- 4 | World Obesity Federation and RTI International. The economic impact of overweight and obesity in 2020 and 2060. https://data.worldobesity.org/publications/WOF-Economic-Impacts-2-V2.pdf. Accessed March 24, 2023.
- 5 | Dang A, Maitra P, Menon N. Labor market engagement and the body mass index of working adults: Evidence from India. Economics and Human Biology. 2019;33:58-77.
- 6 | Kishari P, Mishra CP. Growing menace of fast food consumption in India: time to act. International Journal of Community Medicine and Public Health. 2016;3(6):1355-1362.
- 7 | Law C, Green R, Kadiyala S, et al. Purchase trends of processed foods and beverages in urban India. Global Food Security. 2019;23:191-204.
- 8 | Euromonitor P.L.C. Passport Global Market Information Database. 2014.
- 9 | Aiyar A, Dhingra S, Pingali P. Transitioning to an obese India: Demographic and structural determinants of the rapid rise in overweight incidence 43. 2021;
- 10 | Ramamoorthy T, Kulothungan V, Mathur P. Prevalence and Correlates of Insufficient Physical Activity Among Adults Aged 18-69 Years in India: Findings From the National Noncommunicable Disease Monitoring Survey. J Phys Act Health. 2022;19(3):150-159.
- 11 | Aiyar A, Rahman A, Pingali P. India’s rural transformation and rising obesity burden. World Development. 2021;138
- 12 | Tata-Cornell Institute. Examining the Indian nutrition transition: Reducing the risks for obesity by 2050. https://tci.cornell.edu/?blog=examining-the-indian-nutrition-transition-reducing-the-risks-for-obesity-by-2050. Accessed February 27, 2023.
- 13 | Menon GR, Yadav J, John D. Burden of non-communicable diseases and its associated economic costs in India. Social Sciences and Humanities Open. 2022;5(1)
- 14 | Jeemon P, Mathews E, Jha V. Non-communicable diseases: A modern condition? Nature India. 2019;
- 15 | Menon GR, Singh L, Sharma P, et al. National Burden Estimates of healthy life lost in India, 2017: an analysis using direct mortality data and indirect disability data. The Lancet Global Health. 2019;7(12):e1675-e1684.
- 16 | Kundu MK, Hazra S, Pal S, Bhattacharya M. A review on Noncommunicable Diseases (NCDs) burden, its socio-economic impact and the strategies for prevention and control of NCDs in India. Indian Journal of Public Health 2018;62(4):302-304.
- 17 | Business Group on Health. Global Weight Management Survey. April 7, 2023. https://www.businessgrouphealth.org/resources/global-weight-management-survey. Accessed June 20, 2023.
- 18 | World Health Organization. Mobile technology for preventing NCDs. https://www.who.int/india/health-topics/mobile-technology-for-preventing-ncds. Accessed March 22, 2023.
- 19 | Inoue S, Zimmet P, Caterson I, et al. The Asia-Pacific perspective: Redefining obesity and its treatment. World Health Organization. Regional Office for the Western Pacific. 2000. https://apps.who.int/iris/handle/10665/206936. Accessed December 12, 2022.
- 20 | Deurenberg P, Deurenberg-Yap M, Guricci S. Asians are different from Caucasians and from each other in their body mass index/body fat percent relationship. Obes Rev. 2002;3:141-6.
- 21 | Harvard T.H. Chan School of Public Health. Ethnic Differences in BMI and Disease Risk. https://www.hsph.harvard.edu/obesity-prevention-source/ethnic-differences-in-bmi-and-disease-risk/#References. Accessed March 13, 2023.
- 22 | Misra A, Khurana L. The metabolic syndrome in South Asians: epidemiology, determinants, and prevention. Metab Syndr Relat Disord. 2009;7:497-514.
- 23 | Misra A, Vikram NK. Insulin resistance syndrome (metabolic syndrome) and obesity in Asian Indians: evidence and implications. Nutrition. 2004;20:482-91.
- 24 | Madhu SV, Nitin K, Sambit D, Nishant R, Sanjay K. ESI Clinical Practice Guidelines for the Evaluation and Management of Obesity In India. Indian Journal of Endocrinology and Metabolism. 2022;26(4):295-318.
- 25 | Agrawal P, Gupta K, Mishra V, Agrawal S. The Psychosocial Factors Related to Obesity: A Study Among Overweight, Obese, and Morbidly Obese Women in India. Women Health. 2015;55(6):623-645.
- 26 | Jiwanmall SA, Kattula D, Nandyal MB, et al. Weight Stigma in Patients With Obesity and Its Clinical Correlates: A Perspective From an Indian Bariatric Clinic. Cureus. 2022;14(7)
- 27 | Brewis A, Sreetharan CS, Wutich A. Obesity stigma as a globalizing health challenge. Globalization and Health. 2018;14
- 28 | Business Group on Health. An Employer's Practical Playbook for Treating Obesity. December 5, 2020. https://www.businessgrouphealth.org/resources/managing-overweight-and-obesity-full. Accessed December 12, 2022.
- 29 | Jiwanmall SA, Kattula D, Babajan M, et al. Psychiatric Burden in the Morbidly Obese in Multidisciplinary Bariatric Clinic in South India. Indian Journal of Psychological Medicine. 2018;40(2)
- 30 | Bharati S, Pal M, Hossain G, Bharati P. Effect of Obesity, Socio-Economy and Interactions on Mental Health: A Study of Adolescents in Kolkata, India. Scholarly Journal of Psychology and Behavioral Sciences. 2022;6(1):628=634.
- 31 | Deccan Herald. What IRDAI's order means for mental health coverage in India. https://www.deccanherald.com/business/business-news/what-irdais-order-means-for-mental-health-coverage-in-india-1157925.html. Accessed March 28, 2023.
- 32 | Hindustan Times. Your health insurance plan will cover mental illnesses now, but here's the catch. https://www.hindustantimes.com/india-news/your-health-insurance-plan-will-cover-mental-illnesses-now-but-here-s-the-catch-101666321601282.html. Accessed March 28, 2023.
- 33 | Mittal T, Ahuja A, Dey A, Agarwal S, Goel R. Bariatric and Metabolic Surgery in India: Where Do We Stand? Indian Journal of Surgery 2022;
- 34 | Obesity and Metabolic Surgery Society of India. Guidelines for Bariatric and Metabolic Surgery. https://www.theossi.com/guidelines-obesity-surgery.html. Accessed March 15, 2023.
- 35 | Business Group on Health. Global Weight Management Survey. April 7, 2023. https://www.businessgrouphealth.org/resources/global-weight-management-survey. Accessed June 20, 2023
- 36 | Pramil N Singh, Kristen N Arthur, Michael J Orlich, Wesley James, Anil Purty, Jayakaran S Job, Sujatha Rajaram, Joan Sabaté. Global epidemiology of obesity, vegetarian dietary patterns, and noncommunicable disease in Asian Indians. https://www.sciencedirect.com/science/article/pii/S0002916523048827#:~:text=An%20increase%20in%20noncommunicable%20disease,risk%20factors%20such%20as%20obesity.
This content is for members only. Already a member?
Login
![]()
