February 10, 2023
Inclusion criteria for COE designation will depend on the procedure or service the COE is providing, but there are common metrics that should be assessed across each COE category:
- Adherence to evidence-based approaches to care;
- Success rates for outcomes of care, including at least 1-year post-procedure;
- Meaningful coordination of care with community providers.
- Amount of time needed post-procedure before going back to work;
- Patient satisfaction scores;
- Patient safety metrics;
- Readmission rates;
- Rates of avoided surgeries based on second opinions provided before a procedure is scheduled;
- Predictable costs for an episode of care that are competitive based on the center’s performance on metrics listed above compared to the market; and
- Ancillary services for travel, including support, companion services and post-discharge physical therapy provided at a nearby hotel for patients no longer needing inpatient services but not yet able to travel home.
Condition-Specific Clinical COE Criteria
The Business Group’s guides on cancer and fertility identify specific quality metrics for COEs for those conditions. Employers and their partners should look to national credentialing bodies for condition- or procedure-specific quality metrics.
Additional Considerations for Designations of COEs
- How many facilities will be included in the COE network? Selecting a smaller set of the highest- performing facilities for COE designation can increase the quality of care at those COEs, but this practice may make it more difficult for some employees who live far away to access those facilities.
- Will you rely on health plan COE designations or create your own? Each of the major carriers has COE criteria that are standard in their network design, but self-insured employers may create their own. Creating custom COE criteria requires clinical expertise and additional work to develop and review request for proposals (RFPs), but it can result in designations that better suit individual employer needs. Employers or their consultants should analyze carrier-designated COE performance compared to the market.
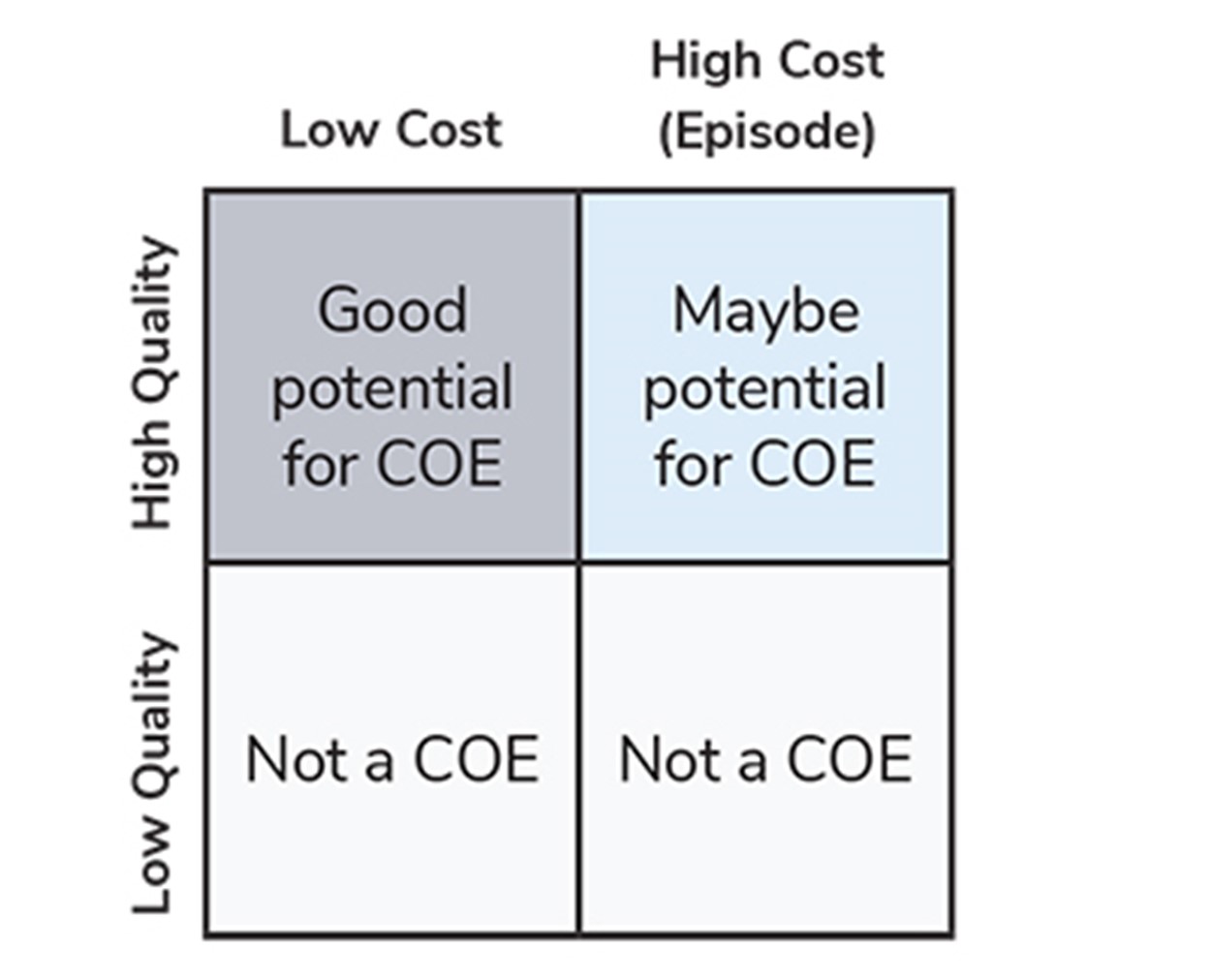
- How important is cost to your COE designation? While low quality is an automatic disqualifier for COE designation, a higher-cost facility may still be worth contracting with as a COE if its quality and outcome metrics are extremely high compared to their competitors (Figure 3).
How Are COEs Reimbursed?
Most COEs are still reimbursed based on a fee-for-service (FFS) basis, but many take on bundled payments that incentivize coordination of care with community providers and create additional predictability in costs over time (Figure 4). Others may take on some risk-sharing or outcomes guarantees. The method of reimbursement is not as important as performance on key outcomes and quality metrics, but it can signify that a health system is willing to take on financial risk and is committed to excellence.
To learn more about value-based care components of COEs, check out the Business Group’s Value-based Purchasing Employer Guide.
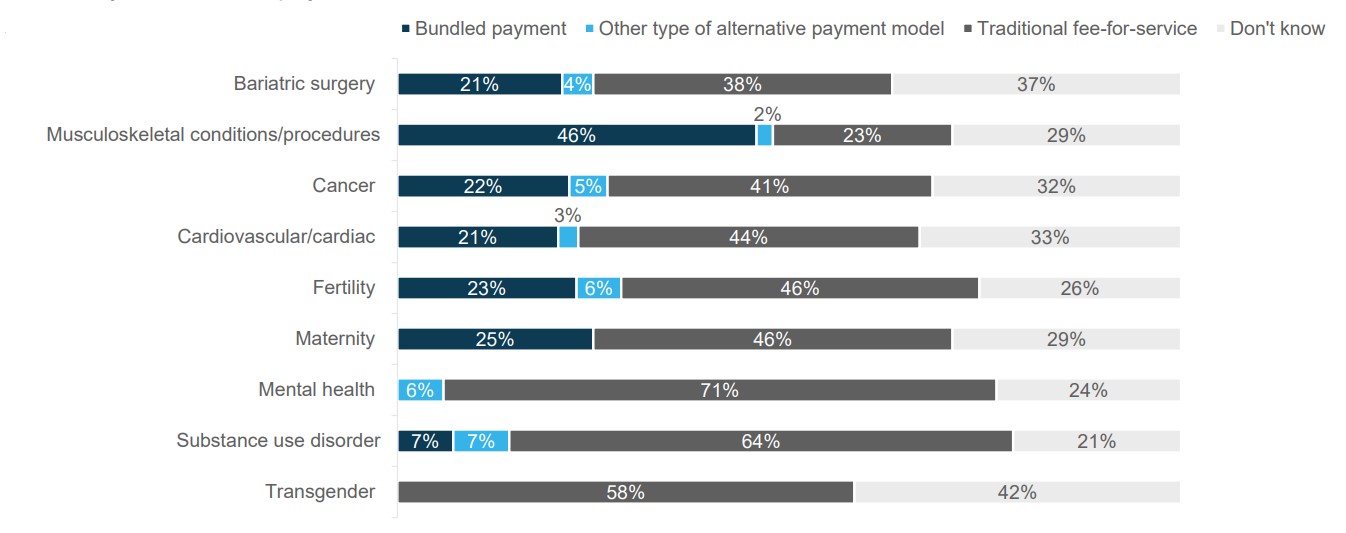
Source: 2021 Large Employers’ Health Care Strategy and Plan Design Survey
How Do You Engage Employees to Use COEs?
There are several steps that employers can take to promote the use of their COE networks to increase appropriate utilization:
-
1 | Identify claims triggers and other indicators that predict that someone will need surgery: The next step is to proactively target communications to them. Claims for physical therapy, for example, can be predictive of a higher likelihood of seeking orthopedic surgery in the future. Therefore, employers and their partners should use this information to reach out to individuals who have submitted such claims to make them aware of the COE program. Other examples of triggers for outreach prior to surgery include:
- Searches for “surgery” or “pain” in price transparency tools;
- Prior authorization requests for surgery at a non-COE provider;
- Physician queries to health plans regarding whether they will be reimbursed for performing a surgery; and
- Plan members calling advocacy services asking if a procedure will be covered.
- 2 | Encourage cross-promotion of COEs by other vendor partners: Concierge, transparency, carrier patient navigators, ACO providers, on-site clinics, employee assistance programs (EAPs) and other vendors should refer patients to COEs when appropriate.
- 3 | Increase benefit for people seeking treatment at a COE: Some employers may waive deductibles and/or provide first-dollar coverage for care at a COE if their plan design allows. Employers that offer a consumer-directed health plan (CDHP) should be aware of limitations on first-dollar coverage for health savings account (HSA)-eligible plans, as the deductible will need to be met prior to this richer benefit kicking in. For many patients seeking treatment at a COE, they will have already met their deductible prior their treatment there, given the cost of diagnostics and other treatment likely leading up to their COE experience. Although less common and incompatible with an HSA, alternative designs using a non-HSA-qualified plan paired with a health reimbursement account (HRA) may permit first-dollar coverage for COEs with more predictable financial exposure for the employer.
- 4 | Limit coverage to COE providers only: This only works if the COE is associated with a travel program, making it available to all employees, or if your COE network provides meaningful geographic access for all employees. This approach drives COE utilization, but it may cause friction for patients seeking care who may not want to travel or would prefer to go to their own doctor.
- 5 | Implement incentives for using a second-opinion program prior to covering certain surgeries or institute penalties to those who do not use those programs. Decision-support or second-opinion programs are sometimes used to direct patients to COEs (Figure 5). A few large employers have had success in dramatically increasing utilization of second-opinion services when penalties are associated with non-use.
- 6 | Provide travel and accommodation support. According to survey results, providing for travel and accommodations is one of the top approaches utilized by large employers to encourage utilization of COEs (Figure 5).
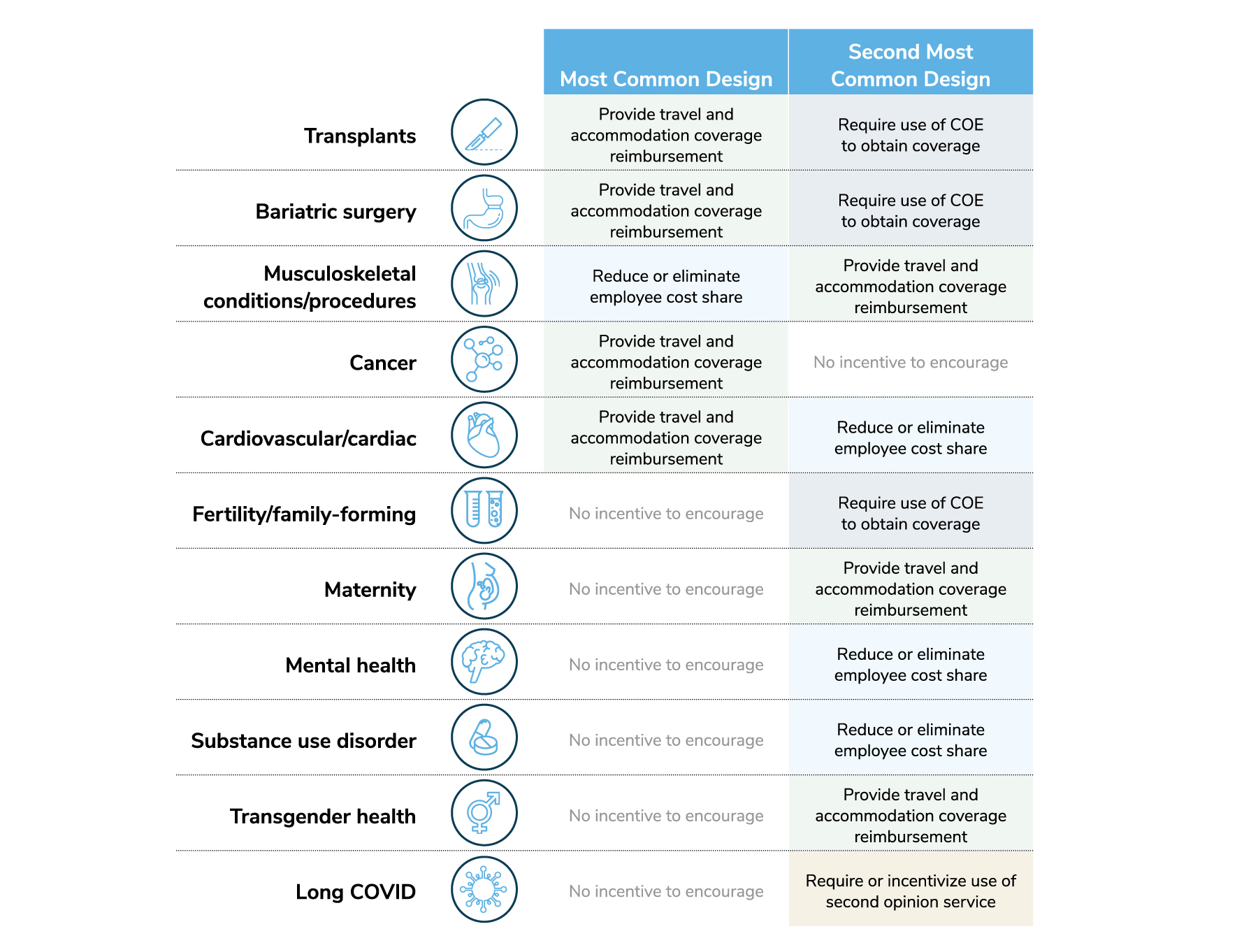
Source: 2023 Large Employers’ Health Care Strategy and Plan Design Survey
More Topics
Articles & Guides- 1 | Marill MC. Raising the stakes to advance equity in Black maternal health. Health Affairs. 2022;41(3):324-330. https://www.healthaffairs.org/doi/10.1377/hlthaff.2022.00036. Accessed December 16, 2022.
- 2 | Hazelden Betty Ford Foundation. Comparing Alcohol and Drug Rehab Success Rates. https://www.hazeldenbettyford.org/about/treatment-success-rates. Accessed December 16, 2022.
This content is for members only. Already a member?
Login
![]()
