February 20, 2023
To deliver on primary care that satisfies the “Principles for an Optimal Primary Care Experience,” employers are asking for the following items from the market. When vendors, including primary care providers themselves, pitch their services to employers, they need to incorporate these elements into their offerings to ensure that they resonate and are considered compelling.
Make Access Easy and On-Demand
![]()
Multiple avenues for people to get care when they need it and where they want it should be present, including brick-and-mortar practices, virtual, chatting and other options. Vendors selling technology to create additional avenues to interact with primary care, such as “smart” symptom checkers, should be integrated into the patient’s primary care ecosystem to support optimal coordination.
Ditch Fee-For-Service
![]()
Reimbursements to providers and systems should move away from fee-for-service or discard it altogether. Optimal primary care does not drive revenue through utilization, but innovation surrounding population health management is only possible when providers are not hamstrung by fee-for-service incentives. Instead, providers should be sharing and benefiting from shared financial risk.
Integrate Mental Health
![]()
A strong integration of mental health care services into primary care interactions should be present. The brain is a part of the body – arguably the most “primary” part – and it needs to be addressed in primary care.
Engage People Before They Become Patients
![]()
Effective primary care must engage patients when they need care for an immediate health concern, but also throughout the year. Effective regular communication helps engage patients to get their preventive screenings and reminds them to go to primary care first when an issue arises. Population health management will require people to think of primary care first when they have a non-emergent health need, but also to engage with their PCP when they’re healthy.
Make Smart Referrals to Expand the Impact of Primary Care
![]()
Referring patients to specialty care based on data, including cost and quality, is a must.
Change Workflows to Improve the Patient and Provider Experience
![]()
Patients shouldn’t have to fight for what they need. Cost, quality and clinical appropriateness information on referrals and prescribing should be integrated into the primary care provider or program’s workflow to make doing the right thing the easy thing for both providers and their patients.
Focus on Continuous Quality Improvement and Report on it
![]()
Tracking outcomes, quality metrics and patient experience scores are necessary for continuous process improvements. This should be reported back to employers regularly.
Help Patients Navigate the System
![]()
An optimal primary care provider group or vendor provides a concierge-like experience for patients, with coaching and navigation support throughout the health care system.
Communicate Your Value
![]()
Across all of these capabilities, primary care vendors providing optimal care must be able to articulate how their approach is unique for the patient and for the employer. The best primary care experience or tool available does no good if no one knows about it or cares to use it.
Drive change with the Health Innovations Forum.
Learn More ![]()
Examples of High-Performing Primary Care Models
What are these primary care models that are making progress toward primary care nirvana? Of course, no one has perfected the practice of medicine and population health management, but several advanced primary care models are improving health outcomes and keeping total costs of care lower than their market competitors. In fact, employer interest in these strategies is increasing, especially in regard to virtual primary care services (Figure 1). But to be effective in driving total cost-of-care reductions, employers must encourage their vendors to make smart referrals to steer patients to high-quality, efficient specialty care. For a more extensive overview of these advanced primary care models and insights on employer strategy for implementation, Business Group on Health members can access the section on primary care in the Value-Based Purchasing Employer Guide.
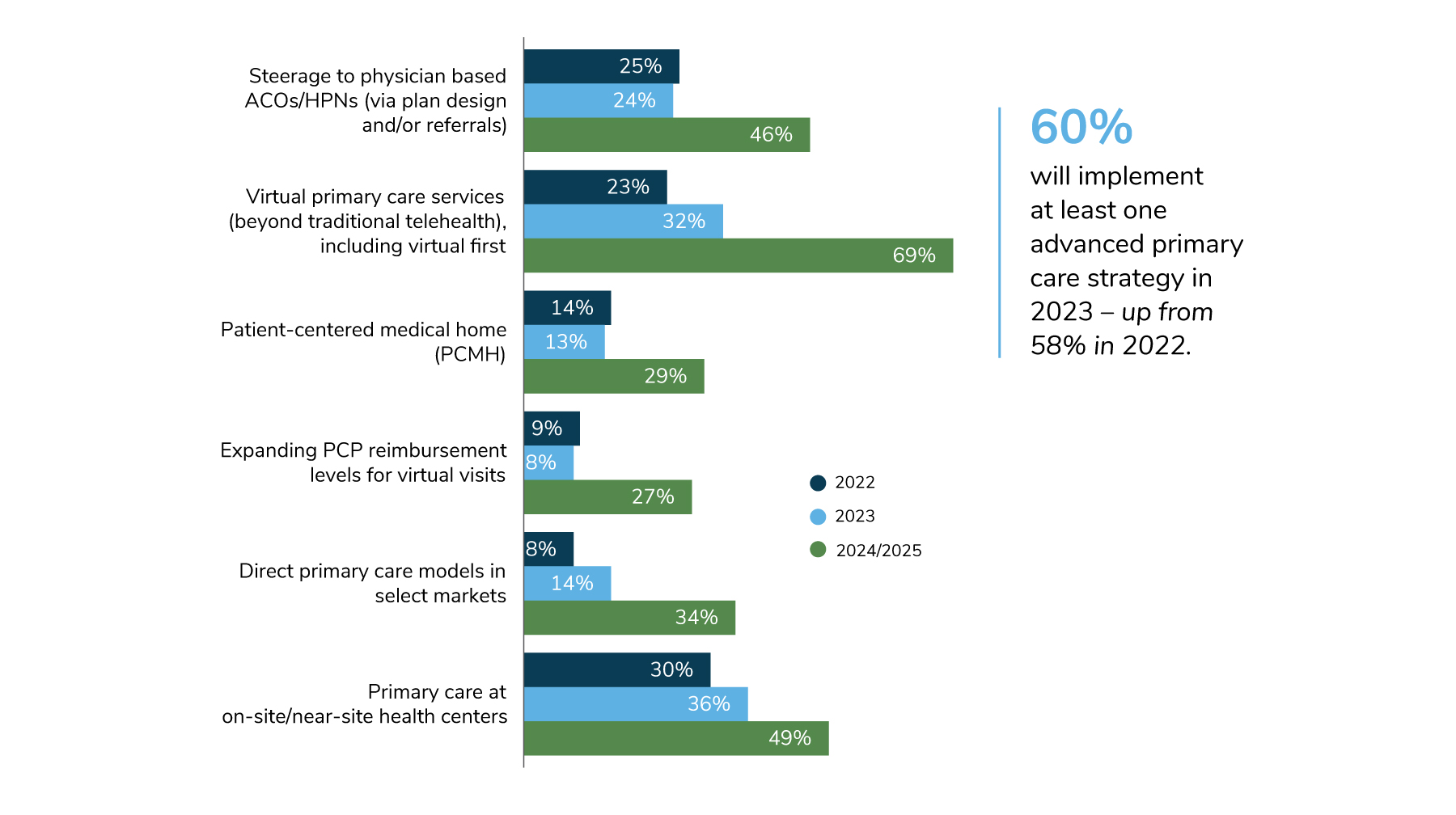
Source: From 2023 Large Employers’ Health Care Strategy and Plan Design Survey. Business Group on Health
Primary Care Focused Accountable Care Organizations (ACOs)
ACOs led by primary care groups have seen greater success in controlling total cost of care in Medicare compared to their counterparts that are run by hospitals. Hospital-led ACOs still generate most of their revenue through inpatient admissions reimbursed through fee-for-service, whereas a primary care group operating under a risk contract can increase their revenue by keeping people healthy and out of the hospital.
Direct Primary Care (DPC)
Practices in the DPC model do not accept fee-for-service payments. In fact, they make no additional revenue each time they see a patient, but instead are paid a per attributed member per month fee to manage the health of their total population. What’s unique about DPC practices is that neither the physicians nor the practices themselves make money for driving utilization. This gives providers the freedom to innovate in how they address population health, because when they keep people healthy and out of more expensive settings of care, everyone “wins” financially.
Enhanced On-Site or Near-Site Clinics with Primary Care
Since on-site and near-site clinics are no longer limited to occupational health, many employers are working with provider partners to increase the scope of services offered in these facilities, including holistic primary care, pharmacy, and mental health. According to the Business Group’s 2023 Large Employers’ Strategy and Plan Design Survey, 36% of respondents are offering primary care at on-site or near-site health centers in 2023—with an additional 13% considering doing so in 2024/2025 (Figure 1). The convenience of having a full suite of primary care services at the worksite saves employees time and increases access to services like mental health care and preventive tests, which are often underutilized. This affords employers a greater ability to drive utilization of high-performing specialty care through virtual referral networks.

Virtual-First Primary Care?
Many brick-and-mortar primary care groups are succeeding in improving access and convenience, as well as reducing costs, by encouraging patients to access them remotely before stepping into the office. But what if you took it a step further and eliminated brick-and-mortar entirely as your primary care “home?” Several established and new players in the telemedicine market are introducing models that migrate the “front door” to primary care to a virtual interaction, with services requiring in-person meetings scheduled separately. These new models are early stage at the moment, but they potentially offer substantial opportunities to increase access and convenience and facilitate efficient referrals to downstream care.
As virtual health continues to expand in the primary care space and more broadly across the health care delivery system, there will be opportunities, barriers and risks that need to be examined and addressed. For further insight on this issue, see Shaping the Future of Virtual Health: Creating Agile Solutions.
