February 26, 2024
Obesity is a complex chronic disease increasing in prevalence worldwide. At the same time, emerging research and therapies are informing new ways to address the escalating epidemic and igniting robust discourse about the treatment of this chronic disease. For employers seeking to align their obesity treatment strategy with the latest evidence, this resource offers information and considerations for creating a comprehensive benefits package, including behavior-based interventions and pharmacological and surgical treatment. It also discusses the role of the workplace environment and culture in supporting employees with obesity on their weight loss journey.
Rates of obesity are rising around the world, including in the United States
According to the most recent data available, 41.9% of U.S. adults have obesity, and by 2030, it’s estimated this number will jump to one in two adults; among those, a quarter will have severe obesity.1,2 These increasing rates extend to children. In 2020, 22.4% of kids ages 2 to 19 had obesity, up from 19.3% in 2019.3 While the reach of obesity is vast, it affects some populations more than others; in the U.S., Black, Indigenous and People of Color (BIPOC) experience higher rates of obesity relative to other groups.2
The negative health effects of obesity are numerous
Obesity is associated with myriad conditions that can reduce quality and length of life. It increases the likelihood of high blood pressure and LDL cholesterol, type 2 diabetes, stroke, osteoarthritis and sleep apnea, to name a few, and in 2018, more than 500,000 people in the U.S. died from causes attributable to overweight and obesity, including cancer, diabetes and cardiovascular disease.4,5 Obesity also increases the risk of poor outcomes from other conditions, including pregnancy and COVID-19.6 For example, research has found that obesity is associated with numerous pregnancy-related complications, as well as a higher risk of maternal mortality compared to pregnant women of a healthy weight.7,8 And as another example, 30.2% of COVID-19 hospitalizations in the U.S. were attributed to obesity from the start of the pandemic through November 2020.9
Beyond the physical health effects of obesity, there is also a relationship between obesity and psychological well-being. A retrospective analysis found that body mass index (BMI) is independently related to health-related quality of life (which includes physical and mental health), with a higher BMI leading to lower quality of life.10
Scientists are also exploring the complicated relationship between obesity and depression, as “research over the past decade has described an intertwined and overlapping biochemical back-and-forth between the two conditions, with each conspiring to aggravate the other.”11 Furthermore, experiencing weight bias or stigma, and then internalizing these negative stereotypes, has been associated with a host of negative mental health outcomes, including depression, anxiety, poor self-esteem and body image.12
Because of its effect on health and well-being, obesity is associated with significant health care spending
As of 2023, obesity ranks among the top ten most expensive chronic diseases for U.S. health care payers.13,14 Higher BMI is associated with increased medical expenditures; one study found $1,800 in excess annual medical costs for individuals with obesity and another showed $2,505 higher annual medical costs for adults with obesity compared to those with a normal weight.15,16 These same studies show annual medical spending associated with obesity ranging from $172 - $260 billion.15,16 Productivity losses are also high; one retrospective study found that compared to normal weight, obesity increases absenteeism 3 days per year due to injury or illness, and the productivity loss from obesity ranged from $13.4 billion to $26.8 billion.17
Rates of obesity are rising worldwide due to multiple and often interrelated factors
Diet, physical activity and sleep, obesogenic environments and social determinants of health, genetics and epigenetics, metabolic adaptation, medications, slowing metabolism, and life events such as menopause and pregnancy all play a role in weight gain (Figure 1.1). Likewise, these factors also make weight loss and weight loss maintenance difficult but not impossible. Beyond these, scientists are studying other contributors to the obesity epidemic, such as the role of ultra-processed foods and the relationship between weight and the gut microbiome, illustrating an evolving and deepening understanding of this chronic condition.18 Both existing and emerging research are important to understanding obesity as a complex disease driven by our biology, environment and behavior, and can help reduce societal weight bias and change obesity treatment paradigms for the better.
Data and research are informing evidence-based ways to treat obesity
Evidence-based treatments include intensive behavioral interventions, anti-obesity medications and bariatric surgery. These treatments represent three pillars of a comprehensive obesity benefit due to research supporting their efficacy; all three should be implemented within the context of a supportive workplace culture.
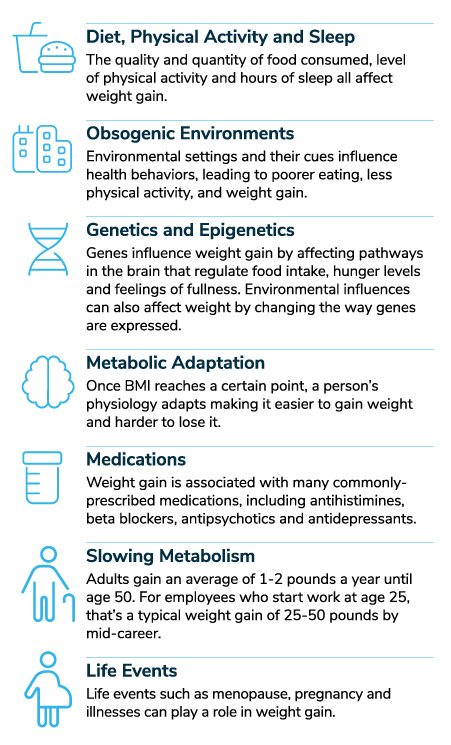
Figure 1.1 Sources:
- 1 | National Institutes of Health. What causes obesity & overweight? July 28, 2021. https://www.nichd.nih.gov/health/topics/obesity/conditioninfo/cause. Accessed January 19, 2024.
- 2 | Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. New England Journal of Medicine. 2017; 376:254-266.
- 3 | World Obesity Federation. The ROOTS of Obesity. https://www.worldobesity.org/what-we-do/our-policy-priorities/the-roots-of-obesity. Accessed January 19, 2024.
- 4 | West, M. What is set point weight theory? Medical News Today. July 14, 2023. https://www.medicalnewstoday.com/articles/set-point-weight. Accessed January 19, 2024.
- 5 | Harvard Health Publishing. Why people become overweight. June 24, 2019. https://www.health.harvard.edu/staying-healthy/why-people-become-overweight. Accessed January 19, 2024.
- 1 | Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. NEJM. 2019;381(25):2440-2450.
- 2 | Centers for Disease Control and Prevention. Adult obesity facts. May 17, 2022. https://www.cdc.gov/obesity/data/adult.html. Accessed October 11, 2023.
- 3 | Lange SJ, Kompaniyets L, Freedman DS, et al. Longitudinal trends in body mass index before and during the COVID-19 pandemic among persons aged 2-19 years - United States, 2018-2020 [published correction appears in MMWR Morb Mortal Wkly Rep. 2021 Sep 24;70(38):1355]. MMWR Morb Mortal Wkly Rep. 2021;70(37):1278-1283.
- 4 | Centers for Disease Control and Prevention. Health effects of overweight and obesity. September 24, 2022. https://www.cdc.gov/healthyweight/effects/index.html. Accessed December 12, 2023.
- 5 | Lopex C, Bendix J, Sagynbekov K. Weighing Down America: 2020 Update. Milken Institute. https://milkeninstitute.org/report/weighing-down-america-2020-update. Accessed June 30, 2022.
- 6 | World Obesity Federation. COVID-19 and Obesity: The 2021 Atlas. https://www.worldobesityday.org/assets/downloads/COVID-19-and-Obesity-The-2021-Atlas.pdf. Accessed August 2022.
- 7 | Frey HA, Ashmead R, Farmer A, et al. Association of prepregnancy body mass index with risk of severe maternal morbidity and mortality among Medicaid neneficiaries. JAMA Network Open. 2022;5(6):e2218986-e2218986.
- 8 | Saucedo M, Esteves-Pereira AP, Pencolé L, et al. Understanding maternal mortality in women with obesity and the role of care they receive: a national case-control study. International Journal of Obesity. 2021;45(1):258-265.
- 9 | Centers for Disease Control and Prevention. Obesity, race/ethnicity, and COVID-19. October 17, 2023. https://www.cdc.gov/obesity/data/obesity-and-covid-19.html. Accessed December 12, 2023.
- 10 | Stephenson J, Smith CM, Kearns B, Haywood A, Bissell P. The association between obesity and quality of life: A retrospective analysis of a large-scale population-based cohort study. BMC Public Health. 2021;21(1):1990.
- 11 | Plackett B. The vicious cycle of depression and obesity. Nature. August 24, 2022. https://www.nature.com/articles/d41586-022-02207-8. Accessed September 21, 2022.
- 12 | Pearl RL, Puhl RM. Weight bias internalization and health: a systematic review. Obesity Reviews. 2018;19(8):1141-1163.
- 13 | Healthpayer Intelligence. Top 10 most expensive chronic diseases for healthcare payers. https://healthpayerintelligence.com/news/top-10-most-expensive-chronic-diseases-for-healthcare-payers. Accessed September 21, 2022.
- 14 | Centers for Disease Control and Prevention. Health and Economic Costs of Chronic Diseases. March 23, 2023. https://www.cdc.gov/chronicdisease/about/costs/index.htm. Accessed October 26, 2023.
- 15 | Cawley J, Biener A, Meyerhoefer C, et al. Direct medical costs of obesity in the United States and the most populous states. J Manag Care Spec Pharm. Mar 2021;27(3):354-366. doi:10.18553/jmcp.2021.20410
- 16 | Ward ZJ, Bleich SN, Long MW, Gortmaker SL. Association of body mass index with health care expenditures in the United States by age and sex. PLoS One. 2021;16(3)
- 17 | Cawley J, Biener A, C M, et al. Job absenteeism costs of obesity in the United States. JOEM. 2021;63(7):565-573.
- 18 | Flam F. Hunger and obesity are the same problem in the US. Bloomberg. October 5, 2022. https://www.bloomberg.com/opinion/articles/2022-10-05/losing-weight-isn-t-as-simple-as-eating-less-and-exercising-more. Accessed October 19, 2022.
More Topics
Articles & Guides-
Part 1An Employer's Practical Playbook for Treating Obesity
-
Executive SummaryRaising the Bar: 6 Ways Employers Can Elevate Their Weight Management Strategy
-
Part 2Intensive Behavioral Interventions
-
Part 3Anti-obesity Medications
-
Part 4Bariatric Surgery
-
Part 5Workplace Culture and Design
-
Part 6Appendix
